Simon
Senior Member
- Messages
- 3,789
- Location
- Monmouth, UK
Book chapter, published March 2015, from "Clinical Challenges in the Biopsychosocial Interface"
Fibromyalgia and Chronic Fatigue: The Underlying Biology and Related Theoretical Issues
Romano G.F.a · Tomassi S.b · Russell A.a · Mondelli V.a · Pariante C.M.a aStress, Psychiatry and Immunology Laboratory, Department of Psychological Medicine, Institute of Psychiatry, King's College London, London, UK
Note the senior author is Prof Carmine Pariente from King's/IoP, which generally champions a biopsychosocial view of mecfs. Pariente is also the lead researcher of a £370k MRC study looking at fatigue following interferon-alpha treatment of Hepatitis C as a model of mecfs, discussed here, lay summaries from here.
Abstract
There is an increasing interest in understanding the biological mechanism underpinning fibromyalgia (FM) and chronic fatigue syndrome (CFS). Despite the presence of mixed findings in this area, a few biological systems have been consistently involved, and the increasing number of studies in the field is encouraging.
This chapter will focus on inflammatory and oxidative stress pathways and on the neuroendocrine system, which have been more commonly examined.
Chronic inflammation, together with raised levels of oxidative stress and mitochondrial dysfunction, has been increasingly associated with the manifestation of symptoms such as pain, fatigue, impaired memory, and depression, which largely characterise at least some patients suffering from CFS and FM.
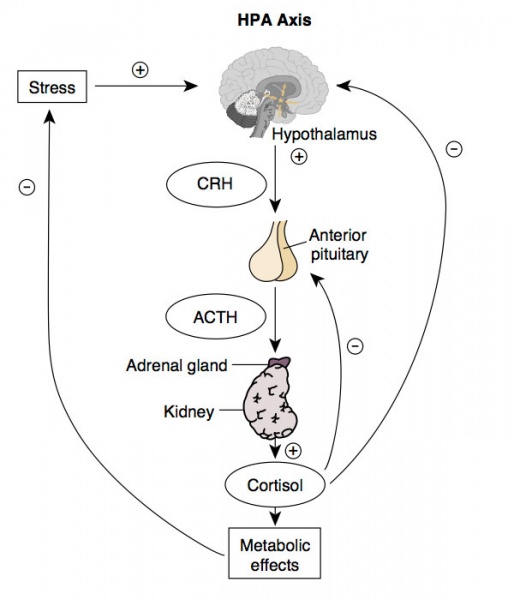
Furthermore, the presence of blunted hypothalamic-pituitary-adrenal axis activity, with reduced cortisol secretion both at baseline and in response to stimulation tests, suggests a role for the hypothalamic-pituitary-adrenal axis and cortisol in the pathogenesis of these syndromes.
However, to what extent these systems' abnormalities could be considered as primary or secondary factors causing FM and CFS has yet to be clarified.
Paywalled, 48-hour access for $12.50 inc UK taxes. You can read some of it at Google books
The articel cites 141 studies, many straight-up biomedical ones. It also explores changes to the HPA,a nd cortisol in particular - and a possible link to childhood trauma. This is a favourire theme at King's. Still, an interesting review. More comments as I have energy (and before my access runs out).
Fibromyalgia and Chronic Fatigue: The Underlying Biology and Related Theoretical Issues
Romano G.F.a · Tomassi S.b · Russell A.a · Mondelli V.a · Pariante C.M.a aStress, Psychiatry and Immunology Laboratory, Department of Psychological Medicine, Institute of Psychiatry, King's College London, London, UK
Note the senior author is Prof Carmine Pariente from King's/IoP, which generally champions a biopsychosocial view of mecfs. Pariente is also the lead researcher of a £370k MRC study looking at fatigue following interferon-alpha treatment of Hepatitis C as a model of mecfs, discussed here, lay summaries from here.
Abstract
There is an increasing interest in understanding the biological mechanism underpinning fibromyalgia (FM) and chronic fatigue syndrome (CFS). Despite the presence of mixed findings in this area, a few biological systems have been consistently involved, and the increasing number of studies in the field is encouraging.
This chapter will focus on inflammatory and oxidative stress pathways and on the neuroendocrine system, which have been more commonly examined.
Chronic inflammation, together with raised levels of oxidative stress and mitochondrial dysfunction, has been increasingly associated with the manifestation of symptoms such as pain, fatigue, impaired memory, and depression, which largely characterise at least some patients suffering from CFS and FM.
Furthermore, the presence of blunted hypothalamic-pituitary-adrenal axis activity, with reduced cortisol secretion both at baseline and in response to stimulation tests, suggests a role for the hypothalamic-pituitary-adrenal axis and cortisol in the pathogenesis of these syndromes.
However, to what extent these systems' abnormalities could be considered as primary or secondary factors causing FM and CFS has yet to be clarified.
Paywalled, 48-hour access for $12.50 inc UK taxes. You can read some of it at Google books
The articel cites 141 studies, many straight-up biomedical ones. It also explores changes to the HPA,a nd cortisol in particular - and a possible link to childhood trauma. This is a favourire theme at King's. Still, an interesting review. More comments as I have energy (and before my access runs out).
Last edited: