ClarkEllis submitted a new blog post:
Dr. Bateman answers IOM questions from the community: Part 1
Clark Ellis brings us Part 1 of an interview with Dr. Lucinda Bateman, where she answered questions posed by the patient community ...
The Institute of Medicine recently published its report into myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). One of the committee members, Dr. Lucinda Bateman, graciously agreed to answer questions submitted by members of the patient community.
Questions were submitted on the Phoenix Rising forum and they can all be viewed here.
Questions have been arranged roughly by topic and will be published in two parts.
This part, the first, covers questions on the committee and IOM process, and the IOM's diagnostic definition.
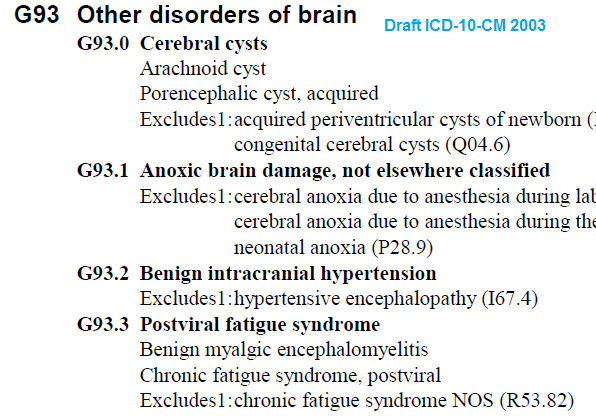
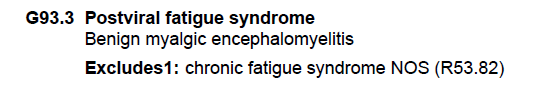
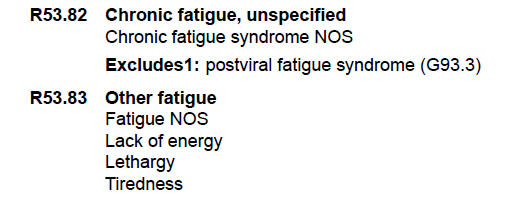
Part 2 will cover the clinicians' guide, the new disease name systemic exertion intolerance disease (SEID) that the IOM has proposed, international classification of diseases (ICD) coding, and miscellaneous topics.
The Committee and the IOM
Q:
When the Department of Health and Human Services contracted the IOM to redefine ME/CFS, it was met with great opposition from the ME/CFS community. Experts, advocates and patients alike wrote letters and voiced their complete opposition against the government creating another criteria when we have a good, proven criteria in the Canadian Consensus Criteria (CCC).
Some of the members of the IOM panel signed the 50 expert letters in opposition of the IOM process. Why did you decide to accept the invitation to serve on the IOM panel when you knew that the community was trying to put a stop to it?
Dr. Bateman:
It's pretty simple. I read the statement of task and changed my mind. For 20 years I have been dreaming about putting together a "think tank" of experts who could critically review what we know and use combined expertise to recommend a path forward. While the IOM contract wasn't exactly what I had envisioned, it had many of the ingredients necessary for success that we haven't had access to — outside experts, staff support and funding. I also felt that the IOM would be able to provide the most "neutral" opinion of the evidence base.
Q:
Has the IOM committee considered soliciting questions about its report via the official IOM ME/CFS website link and posting answers to some or all of the questions that are received from the public on that site?
Dr. Bateman:
I don't think so. The IOM is a non-profit organization that accepts a discreet project or contract, plans and implements the project, creates and publishes a peer review report, and then moves on to a new project. They accepted a massive amount of public input that was considered in the ME/CFS report, a document that now recommends new diagnostic criteria based on the high quality published evidence.
It isn't the responsibility of the IOM to re-evaluate or defend the report based on public comment. The report was a specific task commissioned by DHHS. Now it is peer reviewed published scientific literature that DHHS can utilize to make policy and funding decisions. Most of all, it will serve as an immediate resource for physicians.
Q:
Will the IOM fight and defend their report to physicians who discredit it (often publicly)? What support can we expect? [original wording and context]
Dr. Bateman:
No. The IOM doesn't need to defend the report. It is a summary of the literature based on a standard plan for reviewing the evidence. The recommendations arise directly from the summary of the cited literature, clearly outlined section by section.
The IOM report does challenge physicians and scientists to use what is presented in the report to pursue additional answers about almost all aspects of the illness. The IOM report states clearly that more research and funding are needed, that the report has limitations because the existing evidence base has limitations, and that another funded literature review to revise the diagnostic should be done in no more than 5 years.
There is an expectation that a significant amount of meaningful scientific evidence will be published in the next 3-5 years. I don't know what more we could expect from any academic body.
The Diagnostic Definition
Q:
How confident are you that the sensitivity and specificity of the new criteria are better than any of the other case definitions?
Dr. Bateman:
Sensitivity and specificity must be determined by studies that apply the case definition to patient populations. Obviously, that hasn't been done yet. In my opinion, however, sensitivity and specificity are not well-established for any of the existing case definitions, and the subjective nature of case definition criteria make concrete comparisons a challenge.
Indeed, sensitivity and specificity may be an impossible task when we have subjectively defined and overlapping case definitions. Case definitions are a substitute for diagnosis based on objective diagnostic tests, so the ideal is to move beyond case definitions and toward biomarker discovery that helps us understand pathophysiology and better identify illness subgroups.
The report doesn't make any claims about sensitivity or specificity. The committee's goal was to put the major, persistent, measurable, uniquely combined and previously overlooked symptoms in a simple diagnostic formula that practicing physicians can use to recognize and treat the illness — based on the symptoms reported by patients in multisite studies, backed by research demonstrating the biological basis of the presenting symptoms.
If the diagnostic criteria succeed, and these are indeed a core combination of symptoms, the criteria will have decent sensitivity that is eventually supported by objective markers. If not, the criteria should be revised.
I've heard many complain that the diagnostic criteria don't list exclusionary criteria, and that this will diminish the specificity of the report.
My opinion is the opposite. If physicians are responsible for a differential diagnosis to determine the presence of other conditions, they can't simply order a panel of labs and say they've eliminated other diagnoses. As a clinician who has evaluated and followed hundreds of patients for decades, I can say that the process of differential diagnosis never ends.
It is impossible to list every possible exclusion in diagnostic criteria. Doing so just allows physicians to stop thinking critically about the patient. The IOM report encourages clinicians to make the diagnosis, continue investigations and provide care.
Q:
The IOM diagnostic definition requires that patients have unrefreshing sleep, and that if the symptom is not present at least 50 percent of the time, then the diagnosis of ME/CFS should be questioned. The IOM committee was charged to “develop evidence-based diagnostic criteria for use by clinicians.“ Can you say which study/studies this requirement was derived from? [original wording and context]
Dr. Bateman:
Figure 4-2 in the report (ref: Jason et al., 2013b) shows that 92% of patients in one high-quality study endorsed the symptom "unrefreshing sleep," along with high but sequentially decreasing percentages endorsing "problems falling asleep," "need to nap daily, " problems staying asleep," "waking up early," or sleeping all day/awake all night." When a high frequency (at least 50% of the time) and severity (moderate to severe) were employed, these questions clearly distinguished cases from controls.
In my clinical practice, problems with sleep maintenance plague patients and are often one of the most challenging aspects of treatment. It is amazing to me, that in spite of many sleep studies, whatever the problem with sleep in ME/CFS, it isn't diagnosable by currently used sleep evaluations (polysomnography), based on the published evidence. We need to understand it better.
Q:
Some patients who have ME according to the International Consensus Criteria (ICC) and/or CCC are concerned that they don't fit the criteria for SEID. Is there, or should there be, room for an 'atypical SEID' diagnosis, just as the ICC allowed for an 'atypical ME' diagnosis? [original wording and context]
Dr. Bateman:
Certainly, but I'm not sure that the concern is warranted. All of the SEID criteria are also CCC criteria in one form or another. It is the Fukuda criteria that will prove to be broader than the SEID criteria, leaving many without the diagnosis of CFS, but those are arguably people who don't have ME/CFS anyway. For example, in my clinic that would be people with depression, mild or moderate fibromyalgia, undiagnosed other medical problems, etc.
Q:
Given that a sore throat and tender lymph nodes are often the earliest to appear, why were these symptoms not in the diagnostic criteria? Won't the omission create the risk of patients waiting till other symptoms appear to get a diagnosis, or doctors refusing to diagnose the illness at its earliest stages? [original wording and context]
Dr. Bateman:
The sore throat and tender lymph node criteria aren't present in everyone with ME/CFS, even at onset, and the prevalence of these symptoms diminishes with time. People present to physicians at all stages of illness, not just at onset. Making these symptoms required for diagnosis doesn't make sense. Also, the report states that if these symptoms are present, it supports the diagnosis.
Q:
Currently, patients applying for Social Security Disability Insurance (SSDI) are assessed based on symptoms of the Fukuda criteria, such as palpably swollen lymph nodes, sore throat, muscle tenderness and others. These symptoms are not mandatory for a SEID diagnosis. Did the IOM panel discuss how this new criteria might affect patients seeking disability? [original wording and context]
Dr. Bateman:
Symptoms that are not mandatory are still symptoms that can support the illness. As for the pain symptoms, which can be significant in many patients, especially the severely ill, the diagnosis of comorbid fibromyalgia (widespread hyperalgesia and central sensitization) is often very descriptive and objectively defined.
Q:
Given that muscle weakness/asthenia is a key feature in this illness, why was it not in the diagnostic criteria?
Dr. Bateman:
Actually, while patients feel weak and can have dramatically reduced function, the problem is not exactly muscle weakness by the usual medical definition (hence the “normal” strength exam in most patients). The complaint of weakness or asthenia might be related to abnormal function of the central nervous system, pain, orthostatic intolerance, deconditioning, and PEM, for example. Actual muscle weakness might suggest another diagnosis.
Q:
Unlike the Fukuda, CCC and ICC, the new IOM criteria do not include any exclusions. Dr. Derek Enlander commented to the M.E. Global Chronicle:
"The naiveté of the IOM criteria are the lack of exclusions which are contained in previous criteria. It is peculiar that Lucinda Bateman did not see this problem in her specialist opinion. The IOM criteria as they now stand can include psychiatric induced fatigue or simple fatigue conditions, there are virtually no exclusions."
Can you explain why the panel decided on this move with the risk of including psychiatric conditions? [original wording and context]
Dr. Bateman:
As I discussed above, it is a misconception that the IOM criteria do not require “exclusions” or a differential diagnosis. Physicians are expected to evaluate for other disorders that might completely explain the symptoms, and not make a diagnosis of ME/CFS or SEID if such an illness is identified. The committee decided not to attempt a list of every possible illness that could present with similar symptoms.
It is my own medical opinion that, after routine medical workup has been done (physical exam, ECG, labs, MRIs, mental health screen, etc.), there are very few illnesses, with “normal” tests, that present with such reduced functional capacity, PEM, pervasively disordered sleep, cognitive impairment and orthostatic intolerance. Not depression, for sure.
It would be hard to miss a diagnosis of depression so severe that it caused symptoms resembling ME/CFS. The key is that the combination of core symptoms are mandatory. They must all be present with no other apparent cause after an appropriate medical and mental health workup — a diagnostic process expected of providers.
I’ll also add that people with ME/CFS can and do develop other conditions that contribute to the symptom burden, including depression, menopause, primary sleep disorders and thyroid disorders, for example. Excluding them from an ME/CFS diagnosis would be wrong.
I have many patients that presented with straightforward ME/CFS and went on over the years to develop comorbid conditions which were diagnosed and treated. Don’t they still have ME/CFS?
Q:
The IOM criteria require substantially reduced functional capacity and fatigue, PEM, non-restorative sleep, neurocognitive impairment and/or orthostatic intolerance/ autonomic dysfunction. Does requiring only four criterial symptoms not increase the risk of “including groups of patients that do not suffer from the same disease?"[original wording and context]
Dr. Bateman:
Already answered above.
Q:
Did the IOM panel evaluate whether these diagnostic criteria would be reliable in the diagnosis of the most severe patients who may be bedbound and dependent on caretakers? Put another way, would doctors recognize a severely ill patient as an SEID patient based on the disease description and the criteria provided? [original wording and context]
Dr. Bateman:
The answer is no, the diagnostic criteria were not evaluated for reliability in the most severe patients, because these patients are largely overlooked and not included in the published literature, and the IOM report was generated from this literature. This limitation is recognized and stated in the report, with a call for additional research.
Severely ill patients do have reduced function, activity intolerance, sleep dysregulation, cognitive impairment and orthostatic intolerance. The fact that they have even more symptoms — such as widespread pain and severe central sensitivity — does not preclude a diagnosis using SEID criteria.
Q:
The committee were unable to distinguish between subgroups within ME/CFS, yet by excluding Fukuda CFS patients without PEM from the new diagnostic criteria for ME/CFS, an element of subgrouping was done. My question is in three parts:
a) Did the committee conclude that Fukuda CFS patients without PEM had been misdiagnosed with CFS, and was any consideration given to what will happen to these patients?
Dr. Bateman:
It was recognized that a subgroup, previously diagnosed by Fukuda criteria but without PEM, might be created with the new criteria. In reviewing the existing case definitions, the committee responded to CFS clinicians and patients who communicated strongly that PEM should be a distinguishing feature of ME/CFS, and that it should be a required symptom.
This was supported in the evidence base. As a clinician, I have some ideas about alternate diagnoses for this no-PEM subgroup, but until comparative studies, are done it is only speculation on my part.
Q:
b) In stating that they were unable to distinguish between subgroups and calling for more research, did the committee have a sense that there are subgroups within ME/CFS, but that there was insufficient evidence to identify them at this time?
Dr. Bateman:
Yes.
Q:
c) Did the committee discuss what they felt should happen to Fukuda and Empirical? Did they expect these criteria to be disbanded?
Dr. Bateman:
The IOM committee did not directly address that question or make a recommendation regarding these criteria.
Q:
Was there any discussion of how to evaluate the validity and reliability of these new criteria for this disease prior to roll-out? Same question for the diagnostic tools being recommended if they have not already been evaluated specifically for this disease. If not, shouldn’t that be done before these criteria are rolled out, especially given the lack of recommended biomarkers?
Dr. Bateman:
It was not in the statement of task to do any of those things. The task was to review the literature, and based on the strongest evidence, make recommendations for new diagnostic criteria, on a fairly stringent time schedule. Those tasks are for future research.
Q:
Is SEID intended to cover patients with an existing diagnosis of myalgic encepheomyelits (as described by Dr. Melvin Ramsay and others) and which occurred in outbreaks through the 20th century? Please note, this is not a reference to the CCC or other ME/CFS criteria.
Dr. Bateman:
SEID criteria are intended for current use, for doctors to do better at making the diagnosis in a clinical setting. There was no discussion of anything but using them for this purpose.
Q:
I have had doctors claim in response to the new criteria that all of the symptoms listed there could be psychosomatic or psychological. How would you respond to clinicians who take that view?
Dr. Bateman:
I disagree. The criteria were chosen because they are not only common aspects of illness, but measurable by clinicians and supported by scientific research. Functional decline, disordered sleep, cognitive impairment and orthostatic intolerance are all objective and measurable findings.
We need to improve the tools we use to measure them, but these findings, combined with a typical history and other characteristic symptoms, are how the diagnosis can be made.
Naysayers have always claimed that people with ME/CFS are just experiencing psychological symptoms. That’s nothing new.
Q:
Since it says in the report that the new definition is a clinical one, where does that leave us regarding research criteria? [original wording and context]
Dr. Bateman:
That was and is not the responsibility of the IOM committee to answer.
Q:
The suggested new name indicates that SEID is a systemic illness. But the diagnostic criteria don't include a systemic range of symptoms. Doesn't that contradiction send a confusing message about this disease, to doctors in particular?
Dr. Bateman:
I disagree. Fatigue, reduced function and orthostatic intolerance in particular are each “systemic.” The symptoms in combination create a multisystem illness as well.
A big thank you to Dr. Lucinda Bateman for her answers and willingness to engage with patients.
Thank you also to members of the patient community for taking part and submitting questions. Please note that it was not possible to include every question in the interview, but we included as many as we could.
Some of the questions were shortened or reworded to improve readability of the article and to ensure that we could cover as many questions as possible. In doing so, I tried to maintain the spirit of each question. In such cases, a link to the specific original question has also been provided for full context.
Please also note that if your question did not appear in the interview then that may have been because Dr. Bateman has already provided an answer in her earlier response to an article by Dr. Leonard Jason, or the answer to the question may be evident from the IOM report itself.
Part 2 will be published shortly and will cover the clinicians' guide, the proposed new name: systemic exertion intolerance disease (SEID), international classification of diseases (ICD) coding, and miscellaneous topics.
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
Continue reading the Original Blog Post
Dr. Bateman answers IOM questions from the community: Part 1
Clark Ellis brings us Part 1 of an interview with Dr. Lucinda Bateman, where she answered questions posed by the patient community ...
The Institute of Medicine recently published its report into myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). One of the committee members, Dr. Lucinda Bateman, graciously agreed to answer questions submitted by members of the patient community.
Questions were submitted on the Phoenix Rising forum and they can all be viewed here.
Questions have been arranged roughly by topic and will be published in two parts.
This part, the first, covers questions on the committee and IOM process, and the IOM's diagnostic definition.
Part 2 will cover the clinicians' guide, the new disease name systemic exertion intolerance disease (SEID) that the IOM has proposed, international classification of diseases (ICD) coding, and miscellaneous topics.
The Committee and the IOM
Q:
When the Department of Health and Human Services contracted the IOM to redefine ME/CFS, it was met with great opposition from the ME/CFS community. Experts, advocates and patients alike wrote letters and voiced their complete opposition against the government creating another criteria when we have a good, proven criteria in the Canadian Consensus Criteria (CCC).
Some of the members of the IOM panel signed the 50 expert letters in opposition of the IOM process. Why did you decide to accept the invitation to serve on the IOM panel when you knew that the community was trying to put a stop to it?
Dr. Bateman:
It's pretty simple. I read the statement of task and changed my mind. For 20 years I have been dreaming about putting together a "think tank" of experts who could critically review what we know and use combined expertise to recommend a path forward. While the IOM contract wasn't exactly what I had envisioned, it had many of the ingredients necessary for success that we haven't had access to — outside experts, staff support and funding. I also felt that the IOM would be able to provide the most "neutral" opinion of the evidence base.
Q:
Has the IOM committee considered soliciting questions about its report via the official IOM ME/CFS website link and posting answers to some or all of the questions that are received from the public on that site?
Dr. Bateman:
I don't think so. The IOM is a non-profit organization that accepts a discreet project or contract, plans and implements the project, creates and publishes a peer review report, and then moves on to a new project. They accepted a massive amount of public input that was considered in the ME/CFS report, a document that now recommends new diagnostic criteria based on the high quality published evidence.
It isn't the responsibility of the IOM to re-evaluate or defend the report based on public comment. The report was a specific task commissioned by DHHS. Now it is peer reviewed published scientific literature that DHHS can utilize to make policy and funding decisions. Most of all, it will serve as an immediate resource for physicians.
Q:
Will the IOM fight and defend their report to physicians who discredit it (often publicly)? What support can we expect? [original wording and context]
Dr. Bateman:
No. The IOM doesn't need to defend the report. It is a summary of the literature based on a standard plan for reviewing the evidence. The recommendations arise directly from the summary of the cited literature, clearly outlined section by section.
The IOM report does challenge physicians and scientists to use what is presented in the report to pursue additional answers about almost all aspects of the illness. The IOM report states clearly that more research and funding are needed, that the report has limitations because the existing evidence base has limitations, and that another funded literature review to revise the diagnostic should be done in no more than 5 years.
There is an expectation that a significant amount of meaningful scientific evidence will be published in the next 3-5 years. I don't know what more we could expect from any academic body.
The Diagnostic Definition
Q:
How confident are you that the sensitivity and specificity of the new criteria are better than any of the other case definitions?
Dr. Bateman:
Sensitivity and specificity must be determined by studies that apply the case definition to patient populations. Obviously, that hasn't been done yet. In my opinion, however, sensitivity and specificity are not well-established for any of the existing case definitions, and the subjective nature of case definition criteria make concrete comparisons a challenge.
Indeed, sensitivity and specificity may be an impossible task when we have subjectively defined and overlapping case definitions. Case definitions are a substitute for diagnosis based on objective diagnostic tests, so the ideal is to move beyond case definitions and toward biomarker discovery that helps us understand pathophysiology and better identify illness subgroups.
The report doesn't make any claims about sensitivity or specificity. The committee's goal was to put the major, persistent, measurable, uniquely combined and previously overlooked symptoms in a simple diagnostic formula that practicing physicians can use to recognize and treat the illness — based on the symptoms reported by patients in multisite studies, backed by research demonstrating the biological basis of the presenting symptoms.
If the diagnostic criteria succeed, and these are indeed a core combination of symptoms, the criteria will have decent sensitivity that is eventually supported by objective markers. If not, the criteria should be revised.
I've heard many complain that the diagnostic criteria don't list exclusionary criteria, and that this will diminish the specificity of the report.
My opinion is the opposite. If physicians are responsible for a differential diagnosis to determine the presence of other conditions, they can't simply order a panel of labs and say they've eliminated other diagnoses. As a clinician who has evaluated and followed hundreds of patients for decades, I can say that the process of differential diagnosis never ends.
It is impossible to list every possible exclusion in diagnostic criteria. Doing so just allows physicians to stop thinking critically about the patient. The IOM report encourages clinicians to make the diagnosis, continue investigations and provide care.
Q:
The IOM diagnostic definition requires that patients have unrefreshing sleep, and that if the symptom is not present at least 50 percent of the time, then the diagnosis of ME/CFS should be questioned. The IOM committee was charged to “develop evidence-based diagnostic criteria for use by clinicians.“ Can you say which study/studies this requirement was derived from? [original wording and context]
Dr. Bateman:
Figure 4-2 in the report (ref: Jason et al., 2013b) shows that 92% of patients in one high-quality study endorsed the symptom "unrefreshing sleep," along with high but sequentially decreasing percentages endorsing "problems falling asleep," "need to nap daily, " problems staying asleep," "waking up early," or sleeping all day/awake all night." When a high frequency (at least 50% of the time) and severity (moderate to severe) were employed, these questions clearly distinguished cases from controls.
In my clinical practice, problems with sleep maintenance plague patients and are often one of the most challenging aspects of treatment. It is amazing to me, that in spite of many sleep studies, whatever the problem with sleep in ME/CFS, it isn't diagnosable by currently used sleep evaluations (polysomnography), based on the published evidence. We need to understand it better.
Q:
Some patients who have ME according to the International Consensus Criteria (ICC) and/or CCC are concerned that they don't fit the criteria for SEID. Is there, or should there be, room for an 'atypical SEID' diagnosis, just as the ICC allowed for an 'atypical ME' diagnosis? [original wording and context]
Dr. Bateman:
Certainly, but I'm not sure that the concern is warranted. All of the SEID criteria are also CCC criteria in one form or another. It is the Fukuda criteria that will prove to be broader than the SEID criteria, leaving many without the diagnosis of CFS, but those are arguably people who don't have ME/CFS anyway. For example, in my clinic that would be people with depression, mild or moderate fibromyalgia, undiagnosed other medical problems, etc.
Q:
Given that a sore throat and tender lymph nodes are often the earliest to appear, why were these symptoms not in the diagnostic criteria? Won't the omission create the risk of patients waiting till other symptoms appear to get a diagnosis, or doctors refusing to diagnose the illness at its earliest stages? [original wording and context]
Dr. Bateman:
The sore throat and tender lymph node criteria aren't present in everyone with ME/CFS, even at onset, and the prevalence of these symptoms diminishes with time. People present to physicians at all stages of illness, not just at onset. Making these symptoms required for diagnosis doesn't make sense. Also, the report states that if these symptoms are present, it supports the diagnosis.
Q:
Currently, patients applying for Social Security Disability Insurance (SSDI) are assessed based on symptoms of the Fukuda criteria, such as palpably swollen lymph nodes, sore throat, muscle tenderness and others. These symptoms are not mandatory for a SEID diagnosis. Did the IOM panel discuss how this new criteria might affect patients seeking disability? [original wording and context]
Dr. Bateman:
Symptoms that are not mandatory are still symptoms that can support the illness. As for the pain symptoms, which can be significant in many patients, especially the severely ill, the diagnosis of comorbid fibromyalgia (widespread hyperalgesia and central sensitization) is often very descriptive and objectively defined.
Q:
Given that muscle weakness/asthenia is a key feature in this illness, why was it not in the diagnostic criteria?
Dr. Bateman:
Actually, while patients feel weak and can have dramatically reduced function, the problem is not exactly muscle weakness by the usual medical definition (hence the “normal” strength exam in most patients). The complaint of weakness or asthenia might be related to abnormal function of the central nervous system, pain, orthostatic intolerance, deconditioning, and PEM, for example. Actual muscle weakness might suggest another diagnosis.
Q:
Unlike the Fukuda, CCC and ICC, the new IOM criteria do not include any exclusions. Dr. Derek Enlander commented to the M.E. Global Chronicle:
"The naiveté of the IOM criteria are the lack of exclusions which are contained in previous criteria. It is peculiar that Lucinda Bateman did not see this problem in her specialist opinion. The IOM criteria as they now stand can include psychiatric induced fatigue or simple fatigue conditions, there are virtually no exclusions."
Can you explain why the panel decided on this move with the risk of including psychiatric conditions? [original wording and context]
Dr. Bateman:
As I discussed above, it is a misconception that the IOM criteria do not require “exclusions” or a differential diagnosis. Physicians are expected to evaluate for other disorders that might completely explain the symptoms, and not make a diagnosis of ME/CFS or SEID if such an illness is identified. The committee decided not to attempt a list of every possible illness that could present with similar symptoms.
It is my own medical opinion that, after routine medical workup has been done (physical exam, ECG, labs, MRIs, mental health screen, etc.), there are very few illnesses, with “normal” tests, that present with such reduced functional capacity, PEM, pervasively disordered sleep, cognitive impairment and orthostatic intolerance. Not depression, for sure.
It would be hard to miss a diagnosis of depression so severe that it caused symptoms resembling ME/CFS. The key is that the combination of core symptoms are mandatory. They must all be present with no other apparent cause after an appropriate medical and mental health workup — a diagnostic process expected of providers.
I’ll also add that people with ME/CFS can and do develop other conditions that contribute to the symptom burden, including depression, menopause, primary sleep disorders and thyroid disorders, for example. Excluding them from an ME/CFS diagnosis would be wrong.
I have many patients that presented with straightforward ME/CFS and went on over the years to develop comorbid conditions which were diagnosed and treated. Don’t they still have ME/CFS?
Q:
The IOM criteria require substantially reduced functional capacity and fatigue, PEM, non-restorative sleep, neurocognitive impairment and/or orthostatic intolerance/ autonomic dysfunction. Does requiring only four criterial symptoms not increase the risk of “including groups of patients that do not suffer from the same disease?"[original wording and context]
Dr. Bateman:
Already answered above.
Q:
Did the IOM panel evaluate whether these diagnostic criteria would be reliable in the diagnosis of the most severe patients who may be bedbound and dependent on caretakers? Put another way, would doctors recognize a severely ill patient as an SEID patient based on the disease description and the criteria provided? [original wording and context]
Dr. Bateman:
The answer is no, the diagnostic criteria were not evaluated for reliability in the most severe patients, because these patients are largely overlooked and not included in the published literature, and the IOM report was generated from this literature. This limitation is recognized and stated in the report, with a call for additional research.
Severely ill patients do have reduced function, activity intolerance, sleep dysregulation, cognitive impairment and orthostatic intolerance. The fact that they have even more symptoms — such as widespread pain and severe central sensitivity — does not preclude a diagnosis using SEID criteria.
Q:
The committee were unable to distinguish between subgroups within ME/CFS, yet by excluding Fukuda CFS patients without PEM from the new diagnostic criteria for ME/CFS, an element of subgrouping was done. My question is in three parts:
a) Did the committee conclude that Fukuda CFS patients without PEM had been misdiagnosed with CFS, and was any consideration given to what will happen to these patients?
Dr. Bateman:
It was recognized that a subgroup, previously diagnosed by Fukuda criteria but without PEM, might be created with the new criteria. In reviewing the existing case definitions, the committee responded to CFS clinicians and patients who communicated strongly that PEM should be a distinguishing feature of ME/CFS, and that it should be a required symptom.
This was supported in the evidence base. As a clinician, I have some ideas about alternate diagnoses for this no-PEM subgroup, but until comparative studies, are done it is only speculation on my part.
Q:
b) In stating that they were unable to distinguish between subgroups and calling for more research, did the committee have a sense that there are subgroups within ME/CFS, but that there was insufficient evidence to identify them at this time?
Dr. Bateman:
Yes.
Q:
c) Did the committee discuss what they felt should happen to Fukuda and Empirical? Did they expect these criteria to be disbanded?
Dr. Bateman:
The IOM committee did not directly address that question or make a recommendation regarding these criteria.
Q:
Was there any discussion of how to evaluate the validity and reliability of these new criteria for this disease prior to roll-out? Same question for the diagnostic tools being recommended if they have not already been evaluated specifically for this disease. If not, shouldn’t that be done before these criteria are rolled out, especially given the lack of recommended biomarkers?
Dr. Bateman:
It was not in the statement of task to do any of those things. The task was to review the literature, and based on the strongest evidence, make recommendations for new diagnostic criteria, on a fairly stringent time schedule. Those tasks are for future research.
Q:
Is SEID intended to cover patients with an existing diagnosis of myalgic encepheomyelits (as described by Dr. Melvin Ramsay and others) and which occurred in outbreaks through the 20th century? Please note, this is not a reference to the CCC or other ME/CFS criteria.
Dr. Bateman:
SEID criteria are intended for current use, for doctors to do better at making the diagnosis in a clinical setting. There was no discussion of anything but using them for this purpose.
Q:
I have had doctors claim in response to the new criteria that all of the symptoms listed there could be psychosomatic or psychological. How would you respond to clinicians who take that view?
Dr. Bateman:
I disagree. The criteria were chosen because they are not only common aspects of illness, but measurable by clinicians and supported by scientific research. Functional decline, disordered sleep, cognitive impairment and orthostatic intolerance are all objective and measurable findings.
We need to improve the tools we use to measure them, but these findings, combined with a typical history and other characteristic symptoms, are how the diagnosis can be made.
Naysayers have always claimed that people with ME/CFS are just experiencing psychological symptoms. That’s nothing new.
Q:
Since it says in the report that the new definition is a clinical one, where does that leave us regarding research criteria? [original wording and context]
Dr. Bateman:
That was and is not the responsibility of the IOM committee to answer.
Q:
The suggested new name indicates that SEID is a systemic illness. But the diagnostic criteria don't include a systemic range of symptoms. Doesn't that contradiction send a confusing message about this disease, to doctors in particular?
Dr. Bateman:
I disagree. Fatigue, reduced function and orthostatic intolerance in particular are each “systemic.” The symptoms in combination create a multisystem illness as well.
***************************************************************************************************
A big thank you to Dr. Lucinda Bateman for her answers and willingness to engage with patients.
Thank you also to members of the patient community for taking part and submitting questions. Please note that it was not possible to include every question in the interview, but we included as many as we could.
Some of the questions were shortened or reworded to improve readability of the article and to ensure that we could cover as many questions as possible. In doing so, I tried to maintain the spirit of each question. In such cases, a link to the specific original question has also been provided for full context.
Please also note that if your question did not appear in the interview then that may have been because Dr. Bateman has already provided an answer in her earlier response to an article by Dr. Leonard Jason, or the answer to the question may be evident from the IOM report itself.
Part 2 will be published shortly and will cover the clinicians' guide, the proposed new name: systemic exertion intolerance disease (SEID), international classification of diseases (ICD) coding, and miscellaneous topics.
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
Continue reading the Original Blog Post
Last edited by a moderator: