Okay, it was a pre-registered trial with two groups. 55 people received a group-based intervention - called StreSS - and the other 66 got nothing (told to go back to their GP and s/he would manage them from now on - this was amusingly called "enhanced care").
The StreSS intervention was the standard stuff - first acknowledging their suffering, then challenging patients' "inflexible symptom attributions", identifying "perpetuating thoughts and behaviours", improving "emotional awareness" etc, etc.
The primary outcome measure was based on the SF36, a self-report questionnaire that asks questions about your physical abilities, mental health and overall functioning. They were going to use the PCS score form this scale, which adds up all all the subscales that relate to physical health (vitality, physical functioning, bodily pain, physical role functioning etc), but they changed this after registration to a measure which only include three of the most important physical subscales: physical functioning, bodily pain and vitality.
The StreSS group showed a significantly greater improvement on the primary, self-report measure than the control group. The change to the primary outcome measure didn't make any difference to the results (they presented data for both measures). Most of the secondary measures were mental health measures, and most didn't show significant improvements.
(Edit: forgot to say that the scores on the primary outcome measure declined slightly int he control group over time - so Coyne was right about that part - but conversely, scores in the StreSS group did actually
increase over time, indicating some overall improvement. So its not true that the group differences were entirely driven by deterioration in the control group).
Its interesting to note that they used intention-to-treat, which actually worked in their favour, because more people dropped out in the control group, so had no chance whatsoever of showing even a random improvement.
This is funny:
Schroder paper said:
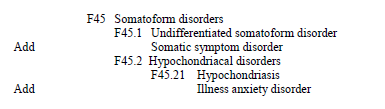
This treatment provides patients with a positive and evidence-based understanding of their
illness that aims to transcend the mind–body dualism inherent in the current diagnostic classifications,and that contrasts with the usual approach to management, which tends to suggest either physical or mental disease.
This treatment was of course based on a heavily dualistic model in which their "minds" were seen as responsible for their physical symptomatoloy.