Extracts from my Dx Revision Watch post:
http://wp.me/pKrrB-3Oe
I am still seeing considerable confusion, misunderstanding and misreporting around
what can and
what cannot be determined from the public version of the ICD-11 Beta drafting platform on emerging proposals for revision of ICD-10′s
Somatoform disorders.
The term
Bodily distress syndrome does not appear in the public version of the ICD-11 Beta drafting platform.
The term entered into the Beta draft is
Bodily distress disorder.
• In September, Oye Gureje, who chairs the
ICD-11 Expert Working Group on Somatic Distress and Dissociative Disorders, will be presenting on
“Proposals and evidence for the ICD-11 classification of Bodily Distress Disorders” as part of a series of ICD-11 Symposia at the World Psychiatric Association’s XVI World Congress, in Madrid.
• There are two working groups advising ICD-11 on the revision of ICD-10′s
Somatoform disorders –
The Primary Care Consultation Group (PCCG);
The ICD-11 Expert Working Group on Somatic Distress and Dissociative Disorders (S3DWG).
• In 2012, the PCCG published a paper proposing a new disorder construct to replace ICD-10-PHC’s F45
“Unexplained somatic symptoms/medically unexplained symptoms” which the group proposed to call
Bodily stress syndrome (BSS) [1].
F48
Neurasthenia was also proposed to be eliminated for the ICD-11-PHC.
• In 2012, the PCCG’s
Bodily stress syndrome category was proposed to sit under a new Mental and behavioural disorder grouping called
Body distress disorders, under which were grouped three other, unrelated disorders, like so:
Extract: Goldberg DP. Comparison Between ICD and DSM Diagnostic Systems for Mental Disorders. In: Sorel E, (Ed.) 21st Century Global Mental Health. Jones & Bartlett Learning, 2012: 37-53 [Free PDF, Sample Chapter Two] [2] Page 51, Table 2.5 The 28 Disorders Proposed for ICD11-PHC (the abridged Primary Care version of ICD-11)
Body distress disorders
15 Bodily stress syndrome [Replaces F45 Unexplained somatic symptoms/medically unexplained symptoms]
16 Acute stress reaction
17 Dissociative disorder
18 Self-harm
[F48 Neurasthenia proposed to be eliminated for ICD11-PHC]
So the PCCG group were proposing the use of a new term,
Body [sic] distress disorders, as a disorder group name for a number of unrelated ICD-11-PHC primary care disorders, whilst proposing the term
Bodily stress syndrome as a new ICD-11-PHC disorder category listed under that group.
[Leaving aside the issue of the current lack of evidence for the validity, reliability and utility of the BSS construct, this presents providers, payers, coders and patients with potentially confusing terminology. Given there is already an operationalized definition and criteria for
Bodily Distress Syndrome, WHO classification experts should have qualms about the potential for confusion between disorder group names and disorder category names, and between proposed disorder names that sound similar to, but which may lack conceptual congruency with similarly named disorders for which definitions and criteria have already been published and which are already in limited use in research and clinical settings.]
• In 2012, the PCCG’s tentative new BSS disorder drew heavily on Fink et al’s
Bodily Distress Syndrome’s (BDS) construct and criteria. Based on physical symptom clusters or patterns from various body systems and (theoretically) on the autonomic arousal or “over-arousal” illness model.
Though not explicit, BSS appeared to have the capacity for capturing the so-called functional somatic syndromes; and in common with BDS, if the symptoms
“were better accounted for by a known physical disease this is not BSS.”
But the tentative BSS criteria also featured some DSM-5 SSD-like psychobehavioural characteristics,
which do not form part of Fink et al’s BDS criteria. There were other, minor criteria discrepancies between BSS and BDS.
• In 2012, the second working group, the S3DWG, also published a paper presenting a new disorder construct which they proposed to call
Bodily distress disorder (BDD) [3]. Again, a similar term to one already in use.
The S3DWG group proposed to subsume all of the ICD-10
Somatoform disorders categories of F45.0 – F45.9, plus F48.0
Neurasthenia, under a new, single BDD disorder category, with a number of severity specifiers (initially, Mild, Moderate and Severe).
• But the S3DWG’s emerging BDD construct was quite different to the PCCG group’s BSS. It was characterized by a simplified criteria set based on excessive preoccupation and psychobehavioural responses to single or multiple, non specific bodily symptoms. The BDD construct shared characteristics with DSM-5′s
Somatic symptom disorder (SSD) – not with Fink et al’s BDS.
• In common with DSM-5′s SSD, the BDD diagnosis eliminated the
“unreliable assumption of causality” and did not exclude the presence of a co-occurring physical health condition. BDD, as described in the 2012 Gureje, Creed paper, and Fink et al’s BDS are divergent constructs.
• So by late 2012, there were
two sets of recommendations – BSS, drawing heavily on Fink’s BDS model, but with a nod towards DSM-5′s SSD, and BDD – with notable similarity to DSM-5′s SSD.
• In early 2012, the disorder name entered into the ICD-11 Beta drafting platform was
Bodily distress disorder, (not
Bodily stress syndrome or
Bodily Distress Syndrome). No Definition for BDD was added at the time.
• In early 2014, a
Definition for
Bodily distress disorder was inserted into the Beta drafting platform. The Definition wording was drawn from the Gureje, Creed (S3DWG) 2012 BDD paper, which had described an SSD-like disorder construct.
• There is currently insufficient evidence in the Beta drafting platform to assert that, in the context of ICD-11 Beta drafting platform, BDD is being defined as a BDS-like construct. The defining BDD characteristics:
high levels of preoccupation regarding bodily symptoms;
unusually frequent or persistent medical help-seeking;
avoidance of normal activities for fear of damaging the body;
are psychological and behavioural responses. Psychological and behavioural responses are not required for Fink et al’s BDS and these characteristics have greater congruency with DSM-5
SSD’s “B type”criteria. There is no evident requirement for symptom patterns or clusters from one or more body systems, as required to meet BDS criteria; examples of BDD symptoms are non specific and patients may be “preoccupied with any bodily symptoms.”
From the limited content displaying in the Beta draft, it simply isn’t possible to determine that BDD, in the context of ICD-11 Beta draft usage, is being defined as a Fink et al BDS-like disorder construct.
•
An additional layer of complexity: recently, the BDD severity specifier
“Severe bodily distress disorder” has been removed from the draft and ICD-10′s
Somatization disorder reinserted.
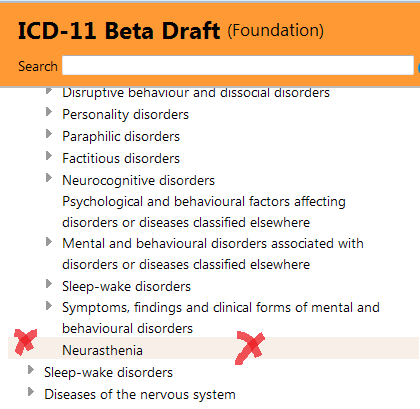
Neurasthenia, previously proposed by both groups to be eliminated or subsumed for ICD-11, has also been inserted back into the Mental and behavioural disorders chapter, which is (currently numbered Chapter 06).
Image source: Chapter 06: Neurasthenia, ICD-11 Beta drafting platform at March 17, 2014
The Definition assigned to
Somatization disorder remains unrevised from legacy text recently imported, unedited, from ICD-10. It is currently unclear how Somatization disorder and Neurasthenia are now intended to integrate within the core ICD-11 and the ICD-11 Primary Care framework, given that a new, single disorder construct had earlier been proposed by both groups to subsume Somatization disorder and all of the ICD-10
Somatoform Disorders categories between F45.0 – F45.9, and to subsume F48.0
Neurasthenia.
No other F45.x categories have been restored to the Beta draft. (There is a reference in the legacy Definition for
Somatization disorder to F45.1
Undifferentiated somatoform disorder but this text has yet to be edited from the text as it had stood under ICD-10′s
Somatoform disorders framework.)
• The development of a replacement for the ICD-10
Somatoform Disorders is a work in progress and proposals may go through several iterations over the next two or three years. The two groups may or may not be striving to reach consensus. The construct favoured by ICD-11 Revision Steering Group may or may not be the construct that is put out for initial field testing.
• Without full disorder descriptions, criteria, inclusions, exclusions, differential diagnoses etc, there is currently insufficient content in the Beta drafting platform to determine the precise nature of whatever construct and criteria is currently favoured by ICD-11 Revision Steering Group; or whether the two groups have reached consensus over a new disorder name and concept; or whether and to what extent the groups’ two (divergent) constructs have been revised since publication of their respective 2012 papers.
Possibly the ICD-11 Symposium IV presentation, later this year, in Madrid, may elucidate. If there is a transcript, summary report or presentation slides of Dr Oye Gureje’s presentation to the World Psychiatric Association XVI World Congress in September, I will post presentation materials, when available. There are some additional notes below the WPA XVI World Congress details.
Notes:
The ICD-11 Primary Care Consultation Group:
The 12 member PCCG leads the development and field testing of the revision of all 28 mental and behavioural disorders proposed for inclusion in the next ICD primary care classification (ICD-11-PHC), an abridged version of the core ICD-11 classification. Per Fink’s colleague, Marianne Rosendal, is a member of the PCCG group.
The members of the PCCG are: SWC Chan, AC Dowell, S Fortes, L Gask, D Goldberg (Chair), KS Jacob, M Klinkman (Vice Chair), TP Lam, JK Mbatia, FA Minhas, G Reed, and M Rosendal.
New disorders that survive the primary care field tests must have an equivalent disorder in the main ICD-11 classification.
The PCCG’s 2012 paper on emerging proposals for BSS and international focus group responses to these tentative proposals can be accessed for free here:
http://fampra.oxfordjournals.org/content/30/1/76.long
http://fampra.oxfordjournals.org/content/30/1/76.full.pdf html
The ICD-11 Expert Working Group on Somatic Distress and Dissociative Disorders:
The second sub working group advising on the revision of ICD-10′s
Somatoform Disorders is the 17 member
Expert Working Group on Somatic Distress and Dissociative Disorders (S3DWG).
The S3DWG is chaired by Prof Oye Gureje.
DSM-5 Somatic Symptom Disorder (SSD) work group member, Prof Francis Creed, is a member of this group. Other than Athula Sumathipala, MD, PhD (UK) and Joan E. Broderick, PhD (Stony Brook University, NY) all other members of this sub working group have yet to be identified. Their names are not listed in the Gureje, Creed 2012 paper [3] and a list of members is not available from the ICD Revision website.
The term entered into the Beta draft is
Bodily distress disorder not
Bodily stress syndrome or
Bodily Distress Syndrome.
Current Definition for Bodily distress disorder, as displaying in the Beta draft at March 16, 2014:
Bodily distress disorder is characterized by high levels of preoccupation regarding bodily symptoms, unusually frequent or persistent medical help-seeking, and avoidance of normal activities for fear of damaging the body. These features are sufficiently persistent and distressing to lead to impairment in personal, family, social, educational, occupational or other important areas of functioning. The most common symptoms include pain (including musculoskeletal and chest pains, backache, headaches), fatigue, gastrointestinal symptoms, and respiratory symptoms, although patients may be preoccupied with any bodily symptoms. Bodily distress disorder most commonly involves multiple bodily symptoms, though some cases involve a single very bothersome symptom (usually pain or fatigue).
This BDD Definition wording is based – in some places verbatim – on the construct descriptions presented in the Gureje, Creed (S3DWG) “Emerging themes…” paper, published in late 2012 [3]. Unfortunately this journal paper remains behind a paywall but I do have a copy.
Extract, Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders. Int Rev Psychiatry. 2012:
“…At the time of preparing this review, a major highlight of the proposals of the S3DWG for the revision of the ICD-10 somatoform disorders is that of subsuming all of the ICD-10 categories of F45.0 – F45.9 and F48.0 under a single category with a new name of ‘bodily distress disorder’ (BDD).
“In the proposal, BDD is defined as ‘A disorder characterized by high levels of preoccupation related to bodily symptoms or fear of having a physical illness with associated distress and impairment. The features include preoccupation with bothersome bodily symptoms and their significance, persistent fears of having or developing a serious illness or unreasonable conviction of having an undetected physical illness, unusually frequent or persistent medical help-seeking and avoidance of normal activities for fear of damaging the body. These features are sufficiently persistent and distressing to lead to impairment of functioning or frequent seeking of reassurance.’”
This 2012 paper goes on to say that the S3DWG’s emerging proposals specify a much simplified set of criteria for a diagnosis of
Bodily distress disorder (BDD) that requires the presence of:
1. High levels of preoccupation with a persistent and bothersome bodily symptom or symptoms; or unreasonable fear, or conviction, of having an undetected physical illness; plus,
2. The bodily symptom(s) or fears about illness are distressing and are associated with impairment of functioning.
And that in doing away with the
“unreliable assumption of its causality” the diagnosis of BDD
“does not exclude the presence of depression or anxiety, or of a co-occurring physical health condition.”
This is not a BDS model – it’s a disorder framework into which
DSM-5′s “Somatic Symptom Disorder” (SSD) could comfortably be integrated, thus smoothing harmonization between ICD-11 and
DSM-5.
(If you want to compare the extent to which the BDS construct and criteria diverges from DSM-5′s SSD construct and criteria, see my graphic
here.)
For the S3DWG’s emerging proposals for BDD, as presented in late 2012, there was no evident requirement for specific symptom counts, or for
BDS-like symptom clusters from one or more body systems. Examples of symptoms are non specific and patients may be
“preoccupied with any bodily symptoms.”
As with DSM-5′s SSD, the focus was not on the number of symptoms, or on symptom patterns or clusters from one or more body systems, or whether symptoms were determined as “medically explained” or “medically unexplained” or of undetermined aetiology, but on the perception of “disproportionate” and “maladaptive” responses to, or “excessive” preoccupation with
any troublesome chronic bodily symptom(s).
So in 2012, the two groups lacked agreement not only over what to call any new, single disorder replacement for ICD-10′s
Somatoform disorders, but also on what disorder construct and criteria should be recommended to ICD Revision.
Given that the wording of the Definition for
Bodily distress disorder as entered into the draft, in January, is based on text from the Gureje, Creed 2012 paper, which had described an SSD-like construct, one might argue that the disorder name and Definition currently displaying in the draft potentially better describes an SSD-like construct – not Fink et al’s BDS.
And with the recent reintroduction into the Beta drafting platform of
Somatization disorder and
Neurasthenia, one might further argue that there is perhaps a recent consideration for a construct that doesn’t veer too far away from the status quo, which could be moulded to accommodate selected of the ICD-10 legacy
Somatoform disorders categories, but which removes the requirement for symptoms to be “medically unexplained” in order that SSD might be shoehorned into an ICD-11 framework for “harmonization” with DSM-5.
But at the moment and in the absence of documentary evidence or clarification by WHO/ICD Revision, what cannot safely be said is that in the context of ICD-11 usage, Bodily distress disorder equates with Fink et al’s Bodily Distress Syndrome.
Caveats: The ICD-11 Beta drafting platform is not a static document: as a work in progress over the next two to three years, it is subject to daily edits and revisions, to field test evaluation and to approval by Topic Advisory Group (TAG) Managing Editors, ICD Revision Steering Group and WHO classification experts.
References:
1. Lam TP, Goldberg DP, Dowell AC, Fortes S, Mbatia JK, Minhas FA, Klinkman MS: Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-11-PHC: an international focus group study.
Fam Pract Feb 2013 [Epub ahead of print July 2012].
Abstract:
http://www.ncbi.nlm.nih.gov/pubmed/22843638
Full free text:
http://fampra.oxfordjournals.org/content/30/1/76.long
PDF:
http://fampra.oxfordjournals.org/content/30/1/76.full.pdf html
2. Goldberg DP. Comparison Between ICD and DSM Diagnostic Systems for Mental Disorders. In: Sorel E, (Ed.) 21st Century Global Mental Health. Jones & Bartlett Learning, 2012: 37-53 [Free PDF, Sample Chapter Two]
http://samples.jbpub.com/9781449627874/Chapter2.pdf
3. Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders.
Int Rev Psychiatry. 2012 Dec;24(6):556-67.
http://www.ncbi.nlm.nih.gov/pubmed/23244611 [Abstract only. Full text behind paywall]
4. ICD-11 Beta drafting platform public version: Bodily distress disorder:
http://apps.who.int/classifications/icd11/browse/f/en#/http://id.who.int/icd/entity/767044268