A.B.
Senior Member
- Messages
- 3,780
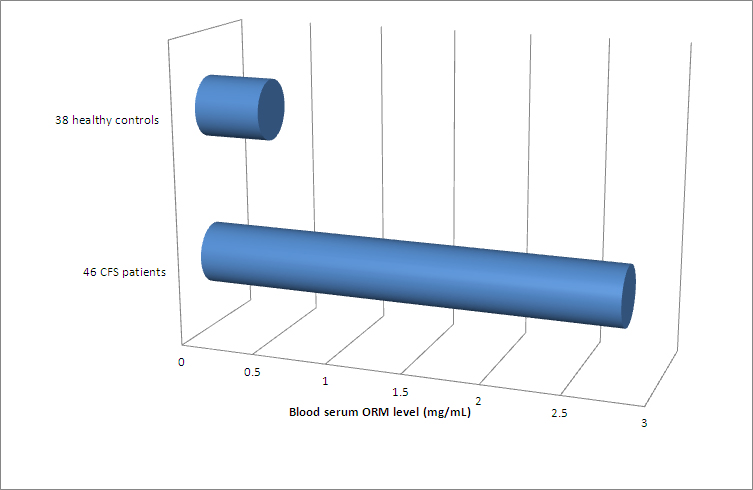
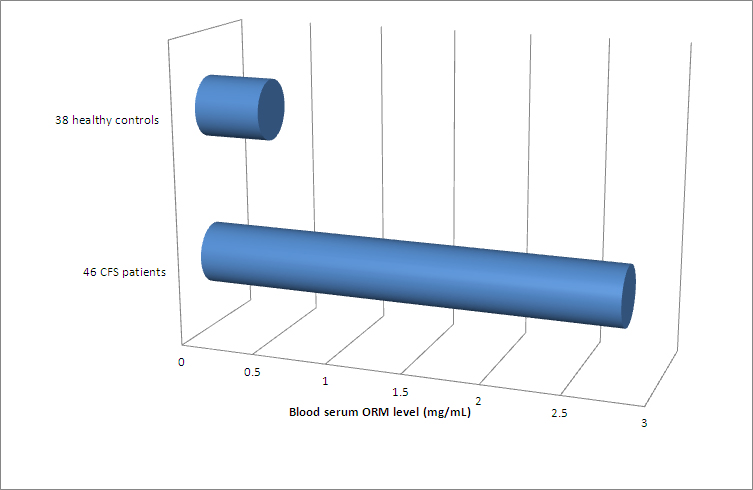
Researchers from China were studying fatigue in an animal model and found an association between fatigue and blood levels of orosomucoid. They then tested CFS patients fulfilling Fukuda criteria and found dramatically increased orosomucoid levels in patients compared to controls.
Orosomucoid is an acute phase protein, increased by inflammation.
There is an article on this here: http://www.meresearch.org.uk/news/orosomucoid-and-mecfs/
Orosomucoid is an acute phase protein, increased by inflammation.
There is an article on this here: http://www.meresearch.org.uk/news/orosomucoid-and-mecfs/
