The model put forward in this 1998 paper has been much cited by the Dutch CBT school and was explicitly used by them as the basis for their version of CBT for CFS. Yet it is a fundamentally flawed piece of work.
The persistence of fatigue in chronic fatigue syndrome and multiple sclerosis: Development of a model, Vercoulen 1998
JHMM Vercoulen, CMA Swanink, OR Hommes, JMD Galama, G Bleijenberg, PJH Jongen, JFM Fennis, and JWM van der Meer
Abstract
Objective. The cause of chronic fatigue syndrome (CFS) is unknown. With respect to factors perpetuating fatigue, on the other hand, a model has been postulated in the literature in which behavioral, cognitive, and affective factors play a role in perpetuating fatigue. In the present study this hypothesized model was tested in patients with CFS and in fatigued patients with multiple sclerosis (MS).
Method. 51 patients with chronic fatigue syndrome and 50 patients with multiple sclerosis matched for age, sex, and education. The hypothesized model was formulated in terms of cause and effect relationships and an integral test of this model was performed by the statistical technique "structural equation modeling".
Results. Attributing complaints to a somatic cause produced low levels of physical activity, which in turn had a causal effect on fatigue severity. In contrast, depression had to be deleted from the model. Two new causal relationships were found: sense of control over symptoms and focusing on bodily symptoms each had a direct causal effect on fatigue. The model showed excellent fit for CFS patients, but was rejected for MS patients. Therefore, a new model for MS patients had to be developed. Sense of control had a causal effect on fatigue. In the MS model no causal relationship was found between the somatic substrate as measured by the Expanded Disability Status Score and fatigue or functional impairment. Causal attributions, low level of physical activity, and focusing on bodily symptoms played an important role in the persistence of fatigue in CFS, but not in MS.
Conclusions. The etiology of CFS is unknown, but the present study shows that cognitive and behavioral factors are involved in the persistence of fatigue. Treatment should be directed at these factors. The processes involved in the subjective experience of fatigue in CFS were different from the processes related to fatigue in MS.
note this abstract come from JHHM Vercoulen's Doctoral Thesis (see Chapter 9) but is just a tiny edit different from the published article so I'm also assuming the paper is not materially changed from the Thesis version.
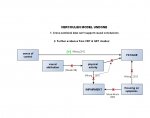
The resulting model looks like this:
There are several fundamental flaws to this stuy:
The persistence of fatigue in chronic fatigue syndrome and multiple sclerosis: Development of a model, Vercoulen 1998
JHMM Vercoulen, CMA Swanink, OR Hommes, JMD Galama, G Bleijenberg, PJH Jongen, JFM Fennis, and JWM van der Meer
Abstract
Objective. The cause of chronic fatigue syndrome (CFS) is unknown. With respect to factors perpetuating fatigue, on the other hand, a model has been postulated in the literature in which behavioral, cognitive, and affective factors play a role in perpetuating fatigue. In the present study this hypothesized model was tested in patients with CFS and in fatigued patients with multiple sclerosis (MS).
Method. 51 patients with chronic fatigue syndrome and 50 patients with multiple sclerosis matched for age, sex, and education. The hypothesized model was formulated in terms of cause and effect relationships and an integral test of this model was performed by the statistical technique "structural equation modeling".
Results. Attributing complaints to a somatic cause produced low levels of physical activity, which in turn had a causal effect on fatigue severity. In contrast, depression had to be deleted from the model. Two new causal relationships were found: sense of control over symptoms and focusing on bodily symptoms each had a direct causal effect on fatigue. The model showed excellent fit for CFS patients, but was rejected for MS patients. Therefore, a new model for MS patients had to be developed. Sense of control had a causal effect on fatigue. In the MS model no causal relationship was found between the somatic substrate as measured by the Expanded Disability Status Score and fatigue or functional impairment. Causal attributions, low level of physical activity, and focusing on bodily symptoms played an important role in the persistence of fatigue in CFS, but not in MS.
Conclusions. The etiology of CFS is unknown, but the present study shows that cognitive and behavioral factors are involved in the persistence of fatigue. Treatment should be directed at these factors. The processes involved in the subjective experience of fatigue in CFS were different from the processes related to fatigue in MS.
note this abstract come from JHHM Vercoulen's Doctoral Thesis (see Chapter 9) but is just a tiny edit different from the published article so I'm also assuming the paper is not materially changed from the Thesis version.
The resulting model looks like this:
There are several fundamental flaws to this stuy:
- This is a cross-sectional study (no 'before' and 'after' data) - and correlation does not mean causation, which is Game Over for the study, really. Still:
- The patients had Oxford-criteria defined CFS and a quarter of them did not have daily fatigue
- Some of the measures eg of 'functional ability' are dubious at best
- The authors hypothesised model failed and they had to modify it 3 separate times before it 'fitted' the data - taking post-hoc chicanery to extremes.