Doing a few more hours of reviewing PubMed studies, I came across “Fecal metagenomic profiles in subgroups of patients with myalgic encephalomyelitis/chronic fatigue syndrome” [2017] There were some interesting findings.
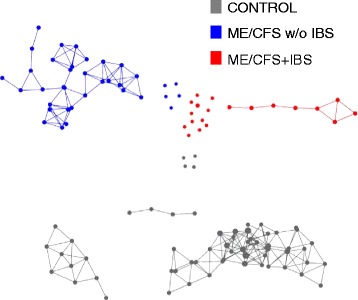
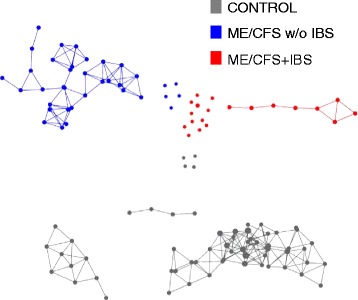 metagenomic profiles
metagenomic profiles
This reinforced my hypothesis that symptoms (and perhaps official diagnosis) are strongly associated with microbiome dysfunction. It reinforces the 1998 study from Australia of microbiome dysfunction.
These reports will be incorporated into the condition profiles which need to be updated to the more sensitive Box-Plot code base.
Increased abundance of unclassified Alistipes and decreased Faecalibacterium emerged as the top biomarkers of ME/CFS with IBS; while increased unclassified Bacteroides abundance and decreased Bacteroides vulgatus were the top biomarkers of ME/CFS without IBS. Despite findings of differences in bacterial taxa and metabolic pathways defining ME/CFS subgroups, decreased metabolic pathways associated with unsaturated fatty acid biosynthesis and increased atrazine degradation pathways were independent of IBS co-morbidity. Increased vitamin B6 biosynthesis/salvage and pyrimidine ribonucleoside degradation were the top metabolic pathways in ME/CFS without IBS as well as in the total ME/CFS cohort. In ME/CFS subgroups, symptom severity measures including pain, fatigue, and reduced motivation were correlated with the abundance of distinct bacterial taxa and metabolic pathways.
The differences in ME/CFS without IBS were driven by the increased abundance of members of Pseudomonadales order, the Clostridiaceae and Pseudomonadaceae family, and the Clostridium, Pseudomonas, Pseudoflavonifractor, Eggerthella, and Coprobacillus genera and the decreased abundance of members of the Dorea genus. The 13 bacterial species driving the differences between the ME/CFS without IBS and control groups were D. formicigenerans, C. catus, and P. distasonis, (all decreased in ME/CFS without IBS) and unclassified Bacteroides, R. gnavus, D. longicatena, P. capillosus, E. lenta, C. symbiosum and scindens, C. bacterium, and Clostridium cf. (all increased in ME/CFS without IBS).
From the prior study (that did not separate with and without IBS), we have:We observed reduced levels of members of the dominant phylum Firmicutes, also noted repeatedly in Crohn’s disease patients [13, 37, 38]. Proteobacteria were more abundant in ME/CFS patients than in controls, observed as well in inflammatory bowel disease (IBD) patients [39, 40].
significantly lower levels of the genus Faecalibacterium, a member of the Ruminococcaceae in the ME/CFS population. For example, Faecalibacterium prausnitzii, which produces an anti-inflammatory protein [45], is reduced in ME/CFS cases relative to controls. …. found a decrease in Bifidobacterium, previously observed in IBS [53–57], IBD [58], and type II diabetes [59]. Bifidobacteria are a group of lactic acid-producing bacteria that are widely used as probiotics and as targets for prebiosis [60]. Treatment with Bifidobacterium infantis 35624 was reported to reduce CRP levels in a cohort of ME/CFS patients [61].
Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome [2016]
Bottom Linesignificantly lower levels of the genus Faecalibacterium, a member of the Ruminococcaceae in the ME/CFS population. For example, Faecalibacterium prausnitzii, which produces an anti-inflammatory protein [45], is reduced in ME/CFS cases relative to controls. …. found a decrease in Bifidobacterium, previously observed in IBS [53–57], IBD [58], and type II diabetes [59]. Bifidobacteria are a group of lactic acid-producing bacteria that are widely used as probiotics and as targets for prebiosis [60]. Treatment with Bifidobacterium infantis 35624 was reported to reduce CRP levels in a cohort of ME/CFS patients [61].
Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome [2016]
This reinforced my hypothesis that symptoms (and perhaps official diagnosis) are strongly associated with microbiome dysfunction. It reinforces the 1998 study from Australia of microbiome dysfunction.
These reports will be incorporated into the condition profiles which need to be updated to the more sensitive Box-Plot code base.
