The title sounded grander than what it actually contained
Open-label pilot for treatment targeting gut dysbiosis in myalgic encephalomyelitis/chronic fatigue syndrome: neuropsychological symptoms and sex comparisons [2018] – Full text
“Conclusions
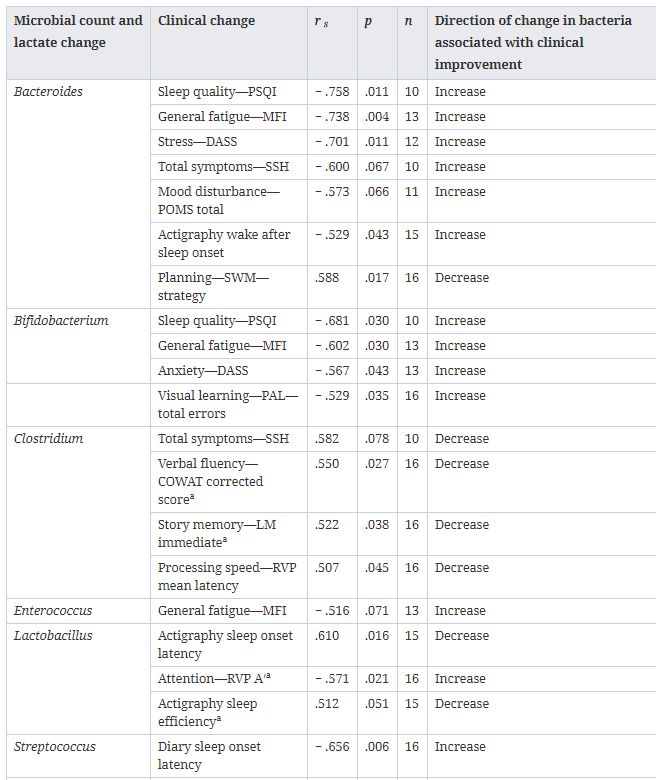
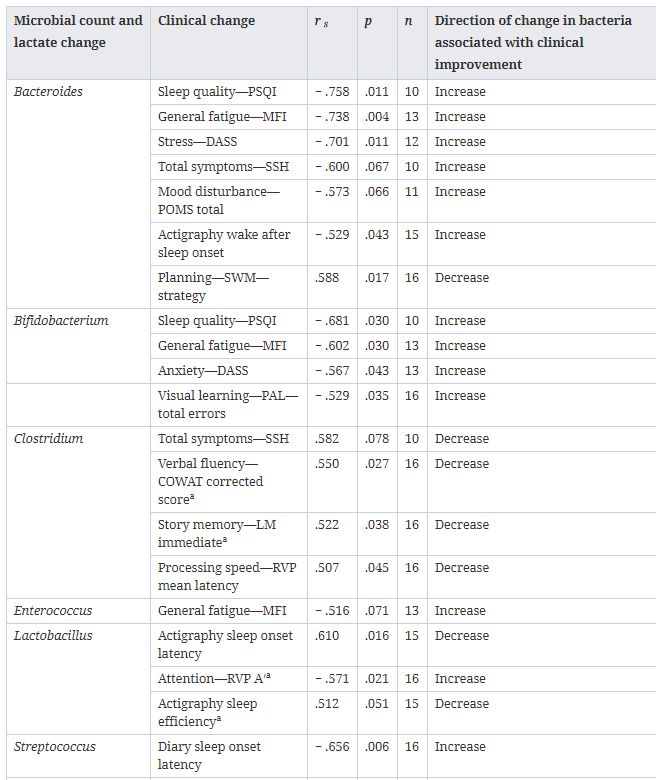
Results support the notion that specific microorganisms interact with some ME/CFS symptoms and offer promise for the therapeutic potential of targeting gut dysbiosis in this population. Streptococcus spp. are not the primary or sole producers of d-lactate. Further investigation of lactate concentrations are needed to elucidate any role of d-lactate in this population. Concurrent microbial shifts that may be associated with clinical improvement (i.e., increased Bacteroides and Bifidobacterium or decreased Clostridium in males) invite enquiry into alternative strategies for individualised treatment.”
The role of staphylococcus was known in 2015, and I did a post on it in January 2016. The d-lactic aspect, I posted about in 2015 in this post Approaches to D-Lactic Acidosis.
What they appear to miss was streptococcus causing histamine issues, see this 2014 post, Histamine intolerance – a possible CFS mechanism.
Their Protocol?
Alternative weeks of:
Antibiotic
Erythromycin
400 mg/b.d.
Probiotic
Pro4-50 d-Lactate Free Multistrain
1 tablet b.d.
It was interesting to note that there was no attempt to reduce streptoccocus by diet etc. The suggestions from existing literature are on the ubiome analysis site. A small example:
Phenotypic and genotypic characterization of antibiotic resistance of methicillin-resistant Staphylococcus aureus isolated from hospital food. [2017]
They did find that shifts of bacteria did result in improvement of symptoms — which is exactly what I expected to see.
Bottom Line
This study supports and illustrates the basics of my model. If you are not too brain fogged, it is an interesting read. Their approach seems a little simplistic, but they did obtain good results.
Open-label pilot for treatment targeting gut dysbiosis in myalgic encephalomyelitis/chronic fatigue syndrome: neuropsychological symptoms and sex comparisons [2018] – Full text
“Conclusions
Results support the notion that specific microorganisms interact with some ME/CFS symptoms and offer promise for the therapeutic potential of targeting gut dysbiosis in this population. Streptococcus spp. are not the primary or sole producers of d-lactate. Further investigation of lactate concentrations are needed to elucidate any role of d-lactate in this population. Concurrent microbial shifts that may be associated with clinical improvement (i.e., increased Bacteroides and Bifidobacterium or decreased Clostridium in males) invite enquiry into alternative strategies for individualised treatment.”
The role of staphylococcus was known in 2015, and I did a post on it in January 2016. The d-lactic aspect, I posted about in 2015 in this post Approaches to D-Lactic Acidosis.
What they appear to miss was streptococcus causing histamine issues, see this 2014 post, Histamine intolerance – a possible CFS mechanism.
Their Protocol?
Alternative weeks of:
Antibiotic
Erythromycin
400 mg/b.d.
Probiotic
Pro4-50 d-Lactate Free Multistrain
1 tablet b.d.
It was interesting to note that there was no attempt to reduce streptoccocus by diet etc. The suggestions from existing literature are on the ubiome analysis site. A small example:
- Bacillus Subtilis [Other things impacted]
- Enterococcus faecium probiotic [Other things impacted]
- Ketogenic diet [Other things impacted]
- Lactobacillus plantarum [Other things impacted]
- Low fat diets [Other things impacted]
- L-Taurine [Other things impacted]
- persimmon tannin [Other things impacted]
- Polymannuronic acid [Other things impacted]
- Walnuts [Other things impacted]
Phenotypic and genotypic characterization of antibiotic resistance of methicillin-resistant Staphylococcus aureus isolated from hospital food. [2017]
- “MRSA strains harbored the highest prevalence of resistance against penicillin (100%), ceftaroline (100%), tetracycline (100%), erythromycin (89.18%) and trimethoprim-sulfamethoxazole
They did find that shifts of bacteria did result in improvement of symptoms — which is exactly what I expected to see.
Bottom Line
This study supports and illustrates the basics of my model. If you are not too brain fogged, it is an interesting read. Their approach seems a little simplistic, but they did obtain good results.
