pattismith
Senior Member
- Messages
- 3,947
@SWAlexander
Although I don't have personnally APSyndrome, I do find useful to take the drugs suggested in this paper (Colchicine, Rapamycin, Ubiquinol). I also take Piroxicam (thromboxan inhibitor)
Targeting thromboinflammation in antiphospholipid syndrome
2022 Netherlandhttps://www.jthjournal.org/article/S1538-7836(22)12803-5/fulltext
Abstract
Antiphospholipid syndrome (APS) is a systemic autoimmune disease, where persistent presence of antiphospholipid antibodies (aPL) leads to thrombotic and obstetric complications.
APS is a paradigmatic thromboinflammatory disease. Thromboinflammation is a pathophysiological mechanism coupling inflammation and thrombosis, which contributes to the pathophysiology of cardiovascular disease.
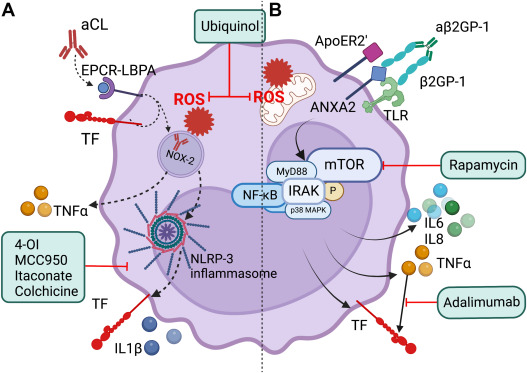
APS can serve as a model to unravel mechanisms of thromboinflammation and the relationship between innate immune cells and thrombosis. Monocytes are activated by aPL into a proinflammatory and procoagulant phenotype, producing proinflammatory cytokines such as tumor necrosis factor α, interleukin 6, as well as tissue factor.
Important cellular signaling pathways involved are the NF-κB-pathway, mammalian target of rapamycin (mTOR) signaling, and the NOD-, LRR-, and pyrin domain-containing protein 3 inflammasome.
All of these may serve as future therapeutic targets.
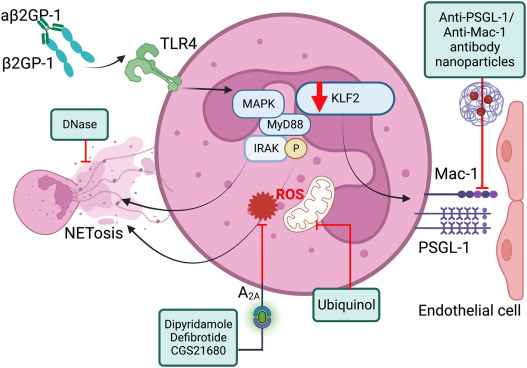
Neutrophils produce neutrophil extracellular traps in response to aPL, and this leads to thrombosis.
Thrombosis in APS also stems from increased interaction of neutrophils with endothelial cells through P-selectin glycoprotein ligand-1. NETosis can be targeted not only with several experimental therapeutics, such as DNase, but also through the redirection of current therapies such as defibrotide and the antiplatelet agent dipyridamole.
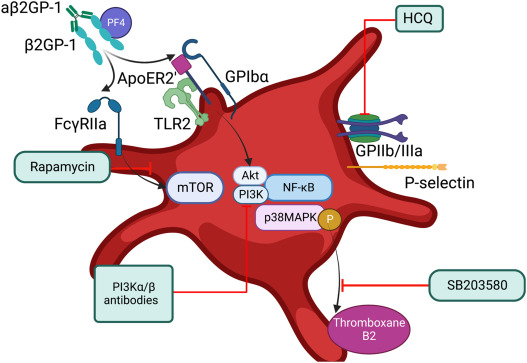
Activation of platelets by aPL leads to a procoagulant phenotype.
Platelet-leukocyte interactions are increased, possibly mediated by increased levels of soluble P-selectin and soluble CD40-ligand. Platelet-directed future treatment options involve the inhibition of several platelet receptors activated by aPL, as well as mTOR inhibition. This review discusses mechanisms underlying thromboinflammation in APS that present targetable therapeutic options, some of which may be generalizable to other thromboinflammatory diseases.