Loss Of Capacity To Recover From Acidosis On Repeat Exercise In Chronic Fatigue Syndrome A Case Control Study
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2362.2011.02567.x/abstract
LOSS OF CAPACITY TO RECOVER FROM ACIDOSIS ON REPEAT EXERCISE IN CHRONIC FATIGUE SYNDROME A CASE CONTROL STUDY
David EJ Jones MD PhD1,, Kieren G Hollingsworth PhD1,2,, Djordje G Jakovljevic PhD3,4,5, Gulnar Fattakhova MD3,4, Jessie Pairman3,4, Andrew M Blamire PhD1,2, Michael I Trenell PhD1,4,5,, Julia L Newton MD PhD3,4,
European Journal of Clinical Investigation 2011 DOI:
10.1111/j.1365-2362.2011.02567.x
Author Information
1Institute of Cellular Medicine
2Newcastle Magnetic Resonance Centre
3Institute for Ageing and Health
4the UK NIHR Biomedical Research Centre in Ageing and Age Related Diseases 5Newcastle Centre for Brain Ageing and Vitality. Newcastle University, UK
*Correspondence: Professor Julia L Newton Institute for Ageing and Health Medical School Framlington Place Newcastle-upon-Tyne NE2 4HH, UK Tel: 0191 2824128 Email: j.l.newton@ncl.ac.uk
Abstract*
Background:?
Chronic fatigue syndrome (CFS) patients frequently describe difficulties with repeat exercise.
Here we explore muscle bioenergetic function in response to 3 bouts of exercise.
Methods:?
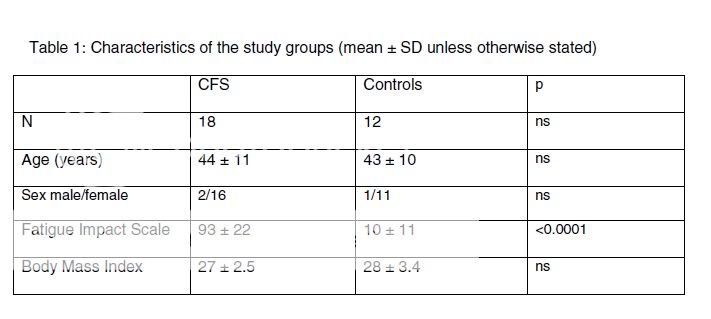
18 CFS (CDC 1994) patients and 12 sedentary controls underwent assessment of maximal voluntary contraction (MVC), repeat exercise with magnetic resonance spectroscopy and cardio-respiratory fitness test to determine anaerobic threshold.
Results:?
CFS patients undertaking MVC fell into 2 distinct groups. 8 (45%) showed normal PCr depletion in response to exercise at 35% of MVC (PCr depletion >33%; lower 95% CI for controls).
10 CFS patients had low PCr depletion (generating abnormally low MVC values).
The CFS whole group exhibited significantly reduced anaerobic threshold, heart rate, VO2, VO2 peak and peak work compared to controls.
Resting muscle pH was similar in controls and both CFS patient groups.
However, the CFS group achieving normal PCr depletion values showed increased intra-muscular acidosis compared to controls after similar work after each of the 3 exercise periods with no apparent reduction in acidosis with repeat exercise of the type reported in normal subjects.
This CFS group also exhibited significant prolongation (almost 4-fold) of the time taken for pH to recover to baseline.
Conclusion:?
When exercising to comparable levels to normal controls CFS patients exhibit profound abnormality in bioenergetic function and response to it.
Although exercise intervention is the logical treatment for patients showing acidosis any trial must exclude subjects who do not initiate exercise as they will not benefit.
This potentially explains previous mixed results in CFS exercise trials.
* I've made each sentence its own paragraph