If ME was down to brain damage, I'd expect we'd have a lot more symptoms of brain damage, and a lot loss symptoms that have nothing to do with the brain. But PEM, muscle aches, swollen lymph nodes, etc, all seem rather peripheral. It would require some serious stretching of biology and logic to tie that into brain function.
-

Welcome to Phoenix Rising!
Created in 2008, Phoenix Rising is the largest and oldest forum dedicated to furthering the understanding of, and finding treatments for, complex chronic illnesses such as chronic fatigue syndrome (ME/CFS), fibromyalgia, long COVID, postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), and allied diseases.
To become a member, simply click the Register button at the top right.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
What if ME is simply brain damage after encephalitis?
- Thread starter silky
- Start date
A.B.
Senior Member
- Messages
- 3,780
If the Rituximab results are confirmed then about 50%, possibly more, have a B cell dependent autoimmune disease. The patients were recruited from neurologists and met the CCC criteria (I hope I remember this right). This autoimmune disease seems to mess up energy metabolism.
That there is little evidence of tissue damage and little signs of inflammation, that complete or nearly complete reovery is possible (with Rituximab or spntaneous remission) all suggest this disease is "functional" in the sense that regulation of normal body processes is disturbed rather than tissue being destroyed.
I think a better word might be "physiological". It's the technical counterpart to "anatomical". "Functional" is pretty loaded, especially in any area where psychobabblers stick their noses... all suggest this disease is "functional" in the sense that regulation of normal body processes is disturbed rather than tissue being destroyed.
Jonathan Edwards
"Gibberish"
- Messages
- 5,256
The complexity of the account is also a huge red flag. This means the theorist had to invoke all kinds of mechanisms to explain the full picture, because none of them on their own "fitted". But if an explanation doesn't fit, we should drop it and look for something else, not pile an extra mechanism on top to deal with its inadequacies.
I beg to differ on this, Woolie.
The reason why rituximab is used for a wide range of autoimmune disease is that I was able to provide a formal demonstration of its efficacy in RA based on a hypothesis that required 55 interconnecting steps. You can give simpler stories but they do not provide an adequate explanation for why the mechanism should run. The RA model was an example of a more general model that predicted that other autoimmune diseases would be just as specific and complex in the way they get going - each one different. Complexity is at the heart of immune function because it provides a feedback control system for vast numbers of overlapping responses.
I had spent twenty years looking for a simple model for RA without luck.
I agree that the imaging studies so far are not convincing. I think they may be looking at the wrong structural level. I think it is very unlikely that there is permanent brain damage in ME of the sort associated with inflammation.
alex3619
Senior Member
- Messages
- 13,810
- Location
- Logan, Queensland, Australia
I wonder about that. I have both symptoms, though only heading toward severe, though my memory issues are mostly with episodic memory, not semantic memory. I have also found other patients who have the same symptoms. I suspect its being ignored. I also suspect its in subgroups.But the profile, its things like severe amnesia, and visual agnosia. That's not really consistent with what we see in MECFS.
alex3619
Senior Member
- Messages
- 13,810
- Location
- Logan, Queensland, Australia
At this point I would only argue for a B cell mediated disease process. It looks like autoimmune or autoinflammatory, but we need more data.If the Rituximab results are confirmed then about 50%, possibly more, have a B cell dependent autoimmune disease.
A.B.
Senior Member
- Messages
- 3,780
At this point I would only argue for a B cell mediated disease process. It looks like autoimmune or autoinflammatory, but we need more data.
In what ways, other than through antibody production or malignancy, could B cells cause disease?
Also, the delayed response to B cell depletion is consistent with an antibody dependent disease process.
That the response time varies quite a bit (from a few months to a year), that symptoms are heterogeneous seems to suggest that this subgroup of ME/CFS involves a variety of antibodies.
Woolie
Senior Member
- Messages
- 3,263
Happy to defer to those who know more on the vagus nerve thing.I beg to differ on this, Woolie.
Last edited:
Woolie
Senior Member
- Messages
- 3,263
Are these visual and memory symptoms more prominent than executive function deficits and working memory problems? For most PwMEs, that's not how it is. The latter two are the first to go, and are affected the worst.I wonder about that. I have both symptoms, though only heading toward severe, though my memory issues are mostly with episodic memory, not semantic memory. I have also found other patients who have the same symptoms. I suspect its being ignored. I also suspect its in subgroups.
Re memory loss, there are various types. There's a medial temporal type of memory loss - characteristic of hypoxia - and that's the kind where someone calls and you don't remember talking to them just a day or so ago, and have the same conversation all over again. Semantic memory for older info is spared, but these people have enormous difficulty learning NEW facts.
Then there's deficits involving controlled, strategic memory. The kind where you struggle to recall particular obscure piece of information about your past or can't remember where you put your sweater after you took it off last Saturday. That sort of memory can be affected by MECFS because is involves high level cognitive control (exec function in older terminologies). You have to conduct a strategic search through your various memories to find the answer. Deficits affecting higher cognitive control are at the center of the typical neuropsyc problems in MECFS.
Still, as you say, you might be atypical.
alex3619
Senior Member
- Messages
- 13,810
- Location
- Logan, Queensland, Australia
Me too, at least for visual issues. Executive function deficits are more severe for me. Working memory is highly variable though. It depends on the day, and sometimes the minute.For most PwMEs, that's not how it is. The latter two are the first to go, and are affected the worst.
Inability to handle math is variable but has been getting worse over the years. I wonder where that fits in the big picture? At my worst even simple counting, like 1,2, 3, is extremely hard or impossible. At my best I find I can occasionally do one or two math calculations if they are simple. I still retain a grasp of mathematical relationships though. During one short remission I regained much of my math in just hours. This is about physiological suppression of brain function in my current opinion, not permanent damage.
On the other hand, while I can recall many of the facts of my life and experiences, I typically cannot recall the experiences themselves. I think its there, its a recall problem.
alex3619
Senior Member
- Messages
- 13,810
- Location
- Logan, Queensland, Australia
Its likely they do, but let me respond with two observations. The first is that B cells might have other functions we do not understand yet. The second is they might cause nothing, but are involved in signalling with the causal processes, probably in other cell types. Remove the signals by removing B cells and you inhibit the problem. We need more data.In what ways, other than through antibody production or malignancy, could B cells cause disease?
The first big step is showing that Rituximab really does work. The second is identifying markers for who might be helped, and what the progression is. With increased clinical use of Rituximab may come increased research interest.
Hmm perhaps a form of lower grade encephalitis takes place in ME that does not always cause fever
I was diagnosed ME much later though my GP was sure it started with the severe adult chicken pox and I had very high fever then.
charles shepherd
Senior Member
- Messages
- 2,239
As a doctor with over 30 years clinical and research involvement with ME/CFS, as well as having personal experience of the illness following a chickenpox encephalitiis, I obviously have a personal interest in whether the pathology of ME involves some form of on-going encephalitic component in the way that most doctors and pathologists understand the term enecephalomyelitis (ie E in ME)
I have reached the conclusion that in our current state of knowledge this is not the case - which is why I believe that encephalopathy is a more appropriate way of describing the E in ME
M encephalopathy is also a far more acceptable term when it comes to a medical profession that is generally unconvinced or even hosile to the name ME
Why the MEA uses the term encephalopathy as well as encephaloymelitis:
http://www.meassociation.org.uk/201...yalgic-encephalopathy-on-the-new-mea-website/
I would add that as a member of the UK post-mortem research group, none of the evidence so far from any of the post-mortems carried out so far has reported neuropathology that equates to an encephalomyelits (ie widepread and significsnt inflammation in brain and spinal cord) being present in ME/CFS
Dr Charles Shepherd
Hon Medical Adviser, MEA
GENERAL INFORMATION ON POST MORTEM RESEARCH AND THE MEA:I am a member of the UK post-mortem research group and the results on some of the post mortems that have been carried out so far have been published - see below
However, none of the post-mortems carried out so far have found the sort of widespread and significant neuroinflammation that would be consistent with an encephalomyelitis (ie inflammation of brain and spinal cord)
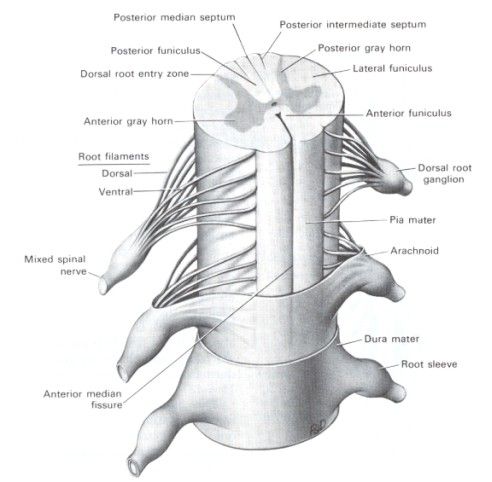
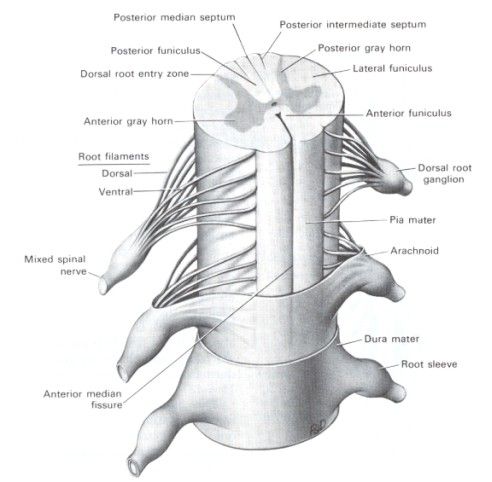
The dorsal root ganglion (where inflammation has been found) form part of the peripheral nervous system
We are continuing to carry out post-mortems when the opportunity arises
DRG: http://www.laesieworks.com/spinal/images-spinal/SpinalCord.jpg
This work is not yet directly linked to the work of the ME Biobank - which is currently only dealing with collection, storage and distribution of blood samples with the anonymised clinical data attached
Pathology of Chronic Fatigue Syndrome: Pilot Study of Four Autopsy Cases
DG O’Donovan1, 2, T Harrower3, S Cader2, LJ Findley2, C Shepherd4, A Chaudhuri2
1Addenbrooke’s Hospital Cambridge UK
2Queen’s Hospital Romford Essex UK
3Royal Devon & Exeter Hospitals UK
4Honorary Medical Advisor to ME Association UK
Chronic Fatigue Syndrome / Myalgic Encephalomyelitis is a disorder characterised by chronic exercise induced fatigue, cognitive dysfunction, sensory disturbances and often pain. The aetiology and pathogenesis are not understood.
We report the post mortem pathology of four cases of CFS diagnosed by specialists.
The causes of death were all unnatural and included: suicidal overdose, renal failure due to lack of food and water, assisted suicide and probable poisoning.
Selected portions of tissue were made available by the various Coroners in the UK and with the assent of the persons in a qualifying relationship.
The cases were 1 male, and 3 female. Ages (years) M32, F32, F43 & F31.
One case showed a vast excess of corpora amylacea in spinal cord and brain of unknown significance but Polyglucosan Body Disease was not supported by clinicopathologial review. No ganglionitis was identified.
One case showed a marked dorsal root ganglionitis and two other cases showed mild excess of lymphocytes with nodules of nageotte in the dorsal root ganglia.
This raises the hypothesis that dysfunction of the sensory and probably also the autonomic nervous system may lead to abnormal neural activity eg hyperalgesia & allodynia rather than anaesthesia and may explain some of the symptoms of CFS / ME such as pain, hypotension, hyperacusis and photophobia. However, the syndrome may be heterogeneous.
Nevertheless, the precise relationship of fatigue, which may be either peripheral or central, to abnormalities in the peripheral nervous system (PNS) needs to be studied.
The differential diagnosis of ganglionitis should be investigated in CFS / ME patients hence Varicella Zoster, Lyme disease, HIV, Sjogren’s disease, paraneoplastic sensory ganglionopathy should be excluded by appropriate history and tests.
Thorough histopathological study of cases coming to autopsy may help to confirm or refute the hypothesis, that CFS is a disease process, and whether the symptomatology may be explained by inflammation of the sensory and autonomic divisions of the PNS.
A specific CFS / ME brain and tissue bank in the UK is proposed.
I have reached the conclusion that in our current state of knowledge this is not the case - which is why I believe that encephalopathy is a more appropriate way of describing the E in ME
M encephalopathy is also a far more acceptable term when it comes to a medical profession that is generally unconvinced or even hosile to the name ME
Why the MEA uses the term encephalopathy as well as encephaloymelitis:
http://www.meassociation.org.uk/201...yalgic-encephalopathy-on-the-new-mea-website/
I would add that as a member of the UK post-mortem research group, none of the evidence so far from any of the post-mortems carried out so far has reported neuropathology that equates to an encephalomyelits (ie widepread and significsnt inflammation in brain and spinal cord) being present in ME/CFS
Dr Charles Shepherd
Hon Medical Adviser, MEA
GENERAL INFORMATION ON POST MORTEM RESEARCH AND THE MEA:I am a member of the UK post-mortem research group and the results on some of the post mortems that have been carried out so far have been published - see below
However, none of the post-mortems carried out so far have found the sort of widespread and significant neuroinflammation that would be consistent with an encephalomyelitis (ie inflammation of brain and spinal cord)
The dorsal root ganglion (where inflammation has been found) form part of the peripheral nervous system
We are continuing to carry out post-mortems when the opportunity arises
DRG: http://www.laesieworks.com/spinal/images-spinal/SpinalCord.jpg
This work is not yet directly linked to the work of the ME Biobank - which is currently only dealing with collection, storage and distribution of blood samples with the anonymised clinical data attached
Pathology of Chronic Fatigue Syndrome: Pilot Study of Four Autopsy Cases
DG O’Donovan1, 2, T Harrower3, S Cader2, LJ Findley2, C Shepherd4, A Chaudhuri2
1Addenbrooke’s Hospital Cambridge UK
2Queen’s Hospital Romford Essex UK
3Royal Devon & Exeter Hospitals UK
4Honorary Medical Advisor to ME Association UK
Chronic Fatigue Syndrome / Myalgic Encephalomyelitis is a disorder characterised by chronic exercise induced fatigue, cognitive dysfunction, sensory disturbances and often pain. The aetiology and pathogenesis are not understood.
We report the post mortem pathology of four cases of CFS diagnosed by specialists.
The causes of death were all unnatural and included: suicidal overdose, renal failure due to lack of food and water, assisted suicide and probable poisoning.
Selected portions of tissue were made available by the various Coroners in the UK and with the assent of the persons in a qualifying relationship.
The cases were 1 male, and 3 female. Ages (years) M32, F32, F43 & F31.
One case showed a vast excess of corpora amylacea in spinal cord and brain of unknown significance but Polyglucosan Body Disease was not supported by clinicopathologial review. No ganglionitis was identified.
One case showed a marked dorsal root ganglionitis and two other cases showed mild excess of lymphocytes with nodules of nageotte in the dorsal root ganglia.
This raises the hypothesis that dysfunction of the sensory and probably also the autonomic nervous system may lead to abnormal neural activity eg hyperalgesia & allodynia rather than anaesthesia and may explain some of the symptoms of CFS / ME such as pain, hypotension, hyperacusis and photophobia. However, the syndrome may be heterogeneous.
Nevertheless, the precise relationship of fatigue, which may be either peripheral or central, to abnormalities in the peripheral nervous system (PNS) needs to be studied.
The differential diagnosis of ganglionitis should be investigated in CFS / ME patients hence Varicella Zoster, Lyme disease, HIV, Sjogren’s disease, paraneoplastic sensory ganglionopathy should be excluded by appropriate history and tests.
Thorough histopathological study of cases coming to autopsy may help to confirm or refute the hypothesis, that CFS is a disease process, and whether the symptomatology may be explained by inflammation of the sensory and autonomic divisions of the PNS.
A specific CFS / ME brain and tissue bank in the UK is proposed.
silky
a gentle soul here to learn
- Messages
- 95
- Location
- Orange County, California
PEM, muscle aches, swollen lymph nodes, etc, all seem rather peripheral. It would require some serious stretching of biology and logic to tie that into brain function
I honestly don't know enough about the brain to say that midbrain or brain stem damage could cause feedback loops resulting in all those symptoms but that was my original hunch. What is your understanding of the etiology?
@silky, are your symptoms very cognitive? I'm wondering how came you to the brain idea in the first place.
I suppose a good definition of cognitive would be useful. I can still reason, and retain much of the vast information I have read since being sick. I can also hold coherent conversations, plan, and visualize. And I can still do mental math
However I am very easily overwhelmed by emotion, or external stimuli. My memory is not as sharp or precise as it once was. And my mental stamina is greatly reduced. Multitasking also feels tortuous, and the speed at which I can think is much slower. Everything generally seems harder
There's also POTS and muscle twitching, which seem neurological if not cognitive. Strangely I do not have marked fluish or immunological symptoms. There is no sore throat or swollen lymph nodes or generally even the malaise / body aches. I'm sure PEM is present but it's probably subtle as I am very very careful not to overextend. Physical stamina is much reduced though strength seems to remain. Luckily I have almost no muscle pain.
I agree that the imaging studies so far are not convincing. I think they may be looking at the wrong structural level. I think it is very unlikely that there is permanent brain damage in ME of the sort associated with inflammation.
Do you think there is any permanent brain damage? Or in your view is it a functional impairment as well?
I have reached the conclusion that in our current state of knowledge this is not the case - which is why I believe that encephalopathy is a more appropriate way of describing the E in ME
So then you would agree with me that the percipitatung cause may be the aftermath of viral brain damage? If so do you think it's impermanent?
charles shepherd
Senior Member
- Messages
- 2,239
I honestly don't know enough about the brain to say that midbrain or brain stem damage could cause feedback loops resulting in all those symptoms but that was my original hunch. What is your understanding of the etiology?
I suppose a good definition of cognitive would be useful. I can still reason, and retain much of the vast information I have read since being sick. I can also hold coherent conversations, plan, and visualize. And I can still do mental math
However I am very easily overwhelmed by emotion, or external stimuli. My memory is not as sharp or precise as it once was. And my mental stamina is greatly reduced. Multitasking also feels tortuous, and the speed at which I can think is much slower. Everything generally seems harder
There's also POTS and muscle twitching, which seem neurological if not cognitive. Strangely I do not have marked fluish or immunological symptoms. There is no sore throat or swollen lymph nodes or generally even the malaise / body aches. I'm sure PEM is present but it's probably subtle as I am very very careful not to overextend. Physical stamina is much reduced though strength seems to remain. Luckily I have almost no muscle pain.
Do you think there is any permanent brain damage? Or in your view is it a functional impairment as well?
So then you would agree with me that the percipitatung cause may be the aftermath of viral brain damage? If so do you think it's impermanent?
In very simple terms, I don't think post infective 'brain damage' is an appropriate term to use in our current state of knowledge
There may well be some form of post infectious neuroinflammation taking place, which would be consistent with research findings which indicate low level immune system activation involving cytokines. And there is some evidence from recent neuroimaging work (especially the research from Japan) to support this type of hypothesis
As ME/CFS symptoms have a great tendency to fluctuate one the course of time, and can improve over time - sometimes to the point of recovery or near recovery, my gut feeling is that we are dealing with an 'upset' to various control centres/thermostats in the brain - rather than some form of permanent brain damage
But we just don't know at the moment - so I would fully accept that there are other hypotheses which could turn out to be correct…
CS
- Messages
- 31
Patient-derived stealth adapted viruses induce illness when inoculated into cats
(https://www.ncbi.nlm.nih.gov/pubmed/8821627). The pathology is systemic, but major manifestations are primarily neurological, including pain, photophobia, and reclusive behavior. The brain differs from other organs of the body in having spatially distributed functions. Consequently, unlike other organs, the brain cannot easily compensate for limited, localized tissue damage by developing heightened activity elsewhere in the organ.
The brain pathology in the inoculated animals is similar to that seen in humans in whom CFS progressed to severe encephalopathy (https://www.ncbi.nlm.nih.gov/pubmed/8856789). There is cellular vacuolization, occasional syncytia and stainable, intracellular and extracellular materials (ACE pigments).
The inoculated animals clinically recover from their illness in spite of there being no inflammation.
(https://www.ncbi.nlm.nih.gov/pubmed/8821627). The pathology is systemic, but major manifestations are primarily neurological, including pain, photophobia, and reclusive behavior. The brain differs from other organs of the body in having spatially distributed functions. Consequently, unlike other organs, the brain cannot easily compensate for limited, localized tissue damage by developing heightened activity elsewhere in the organ.
The brain pathology in the inoculated animals is similar to that seen in humans in whom CFS progressed to severe encephalopathy (https://www.ncbi.nlm.nih.gov/pubmed/8856789). There is cellular vacuolization, occasional syncytia and stainable, intracellular and extracellular materials (ACE pigments).
The inoculated animals clinically recover from their illness in spite of there being no inflammation.
jimells
Senior Member
- Messages
- 2,009
- Location
- northern Maine
Hmmm, 74 posts and not one mention of Naviaux's Cell Danger Response theory. I wonder why?
I have found his model to be very useful in understanding my own illness and what causes most (all?) of my symptoms secondary to the core inability to sustain activity. Extracellular ATP is the key.
After ten years of sometimes severe POTS crashes, I now have a successful treatment plan for POTS: two anti-histamines taken daily, and an alpha blocker and a beta blocker as "rescue meds" when histamine overwhelms the anti-histamines. For me, this treatment is substantially more effective than IV saline.
I think I can demonstrate through my own experience of the illness and the available research literature that extracellular ATP is causing widespread activation of mast cells, leading directly to hyperadrenergic POTS, orthostatic hypotension (yes I have both, but not at the same time), IBS, Reynauds syndrome, cognitive difficulties, widespread itching, and even temperature instability.
I'm pretty sure that my mast cells are sometimes activated by standing up, and probably just by waking up, as mast cells can be activated by corticotropin-releasing hormone (CRH). For example, every morning I wake up with orthostatic hypotension. Two hours later, it is gone, once the morning dump of histamine is metabolized and/or blocked by the anti-histamine.
So my question to the group is, why is there so little interest in a possible role for mast cells in ME, here on the forum as well as among researchers?
Often seen, rarely recognized: mast cell activation disease--a guide to diagnosis and therapeutic options
The role of mast cells in functional GI disorders
Hyperadrenergic postural tachycardia syndrome in mast cell activation disorders
Frontline Science: Corticotropin-releasing factor receptor subtype 1 is a critical modulator of mast cell degranulation and stress-induced pathophysiology.
I have found his model to be very useful in understanding my own illness and what causes most (all?) of my symptoms secondary to the core inability to sustain activity. Extracellular ATP is the key.
After ten years of sometimes severe POTS crashes, I now have a successful treatment plan for POTS: two anti-histamines taken daily, and an alpha blocker and a beta blocker as "rescue meds" when histamine overwhelms the anti-histamines. For me, this treatment is substantially more effective than IV saline.
I think I can demonstrate through my own experience of the illness and the available research literature that extracellular ATP is causing widespread activation of mast cells, leading directly to hyperadrenergic POTS, orthostatic hypotension (yes I have both, but not at the same time), IBS, Reynauds syndrome, cognitive difficulties, widespread itching, and even temperature instability.
I'm pretty sure that my mast cells are sometimes activated by standing up, and probably just by waking up, as mast cells can be activated by corticotropin-releasing hormone (CRH). For example, every morning I wake up with orthostatic hypotension. Two hours later, it is gone, once the morning dump of histamine is metabolized and/or blocked by the anti-histamine.
So my question to the group is, why is there so little interest in a possible role for mast cells in ME, here on the forum as well as among researchers?
Often seen, rarely recognized: mast cell activation disease--a guide to diagnosis and therapeutic options
The role of mast cells in functional GI disorders
Hyperadrenergic postural tachycardia syndrome in mast cell activation disorders
Frontline Science: Corticotropin-releasing factor receptor subtype 1 is a critical modulator of mast cell degranulation and stress-induced pathophysiology.
Last edited:
charles shepherd
Senior Member
- Messages
- 2,239
I honestly don't know enough about the brain to say that midbrain or brain stem damage could cause feedback loops resulting in all those symptoms but that was my original hunch. What is your understanding of the etiology?
I suppose a good definition of cognitive would be useful. I can still reason, and retain much of the vast information I have read since being sick. I can also hold coherent conversations, plan, and visualize. And I can still do mental math
However I am very easily overwhelmed by emotion, or external stimuli. My memory is not as sharp or precise as it once was. And my mental stamina is greatly reduced. Multitasking also feels tortuous, and the speed at which I can think is much slower. Everything generally seems harder
There's also POTS and muscle twitching, which seem neurological if not cognitive. Strangely I do not have marked fluish or immunological symptoms. There is no sore throat or swollen lymph nodes or generally even the malaise / body aches. I'm sure PEM is present but it's probably subtle as I am very very careful not to overextend. Physical stamina is much reduced though strength seems to remain. Luckily I have almost no muscle pain.
Do you think there is any permanent brain damage? Or in your view is it a functional impairment as well?
So then you would agree with me that the percipitatung cause may be the aftermath of viral brain damage? If so do you think it's impermanent?
As before, I would NOT want to use the rather emotive term 'brain damage' - which implies a permanent and significant structural damage to the brain
But I do think we may be dealing with the consequence of some form of low level neuroinflammation - as can occur in a range of infective and inflammatory medical conditions (e.g. HIV, SLE)
CS
silky
a gentle soul here to learn
- Messages
- 95
- Location
- Orange County, California
The inoculated animals clinically recover from their illness in spite of there being no inflammation
What do you think contributes to the animals' recovery?
Hmmm, 74 posts and not one mention of Naviaux's Cell Danger Response theory. I wonder why?
I really respect and admire Dr Naviaux and think his metabolic work is groundbreaking. But I don't see what solid evidence he has that a cell danger response exists other than the metabolic links he's drawn to c elegans. To me his theory seems to be one of many that could explain the symptoms. We know brain injury is real and can have systemic effects, we don't yet know if the cell danger response exists (at least that is my understanding). I would prefer that Dr Naviaux is right though, and that a drug like suramin could flip the switch and bring back everything including the brain.
I am really interested in how you treated your POTS. Is it completely gone now?
And how did you draw the links between extracellular ATP, mast cells, and POTS?
I have wondered about mast cells but I do not have allergic reactions
As before, I would NOT want to use the rather emotive term 'brain damage' - which implies a permanent and significant structural damage to the brain
Point taken
Dr Shepherd, my understanding is that you yourself recovered from ME. Were your cognitive symptoms severe?