undiagnosed
Senior Member
- Messages
- 246
- Location
- United States
My health has been deteriorating with new issues compounding at a seemingly exponential rate. I don't have a diagnosis and don't meet the CFS criteria but am looking for advice in case anyone has had similar issues. I am not really getting anywhere with doctors which is very frustrating. For context, I'm a 28 year old male with a BMI of 20.3, not taking any medications.
I have had a number of lab tests done which resulted in a couple results outside the reference range and a number of results approaching the limits. Table 1 shows all lab results that were in the bottom 10% of the reference range. The Percent column was calculated using the CDF assuming a normal distribution with a 95% reference interval. Therefore 2.5% represents the lower reference interval limit.
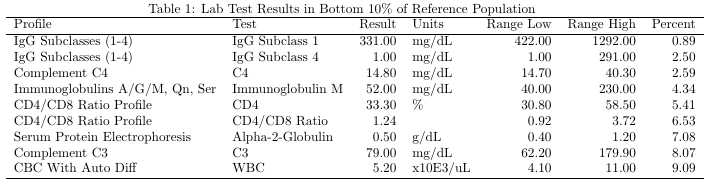
IgG Subclass 1 is below the reference interval and in the bottom 0.89% of the reference population. I recently discovered this deficiency and am not sure if it would affect antibody production and invalidate the results of previous antibody tests. I am concerned about the possibility though. As can be seen, a number of other immune system related markers are approaching the lower limits as well.
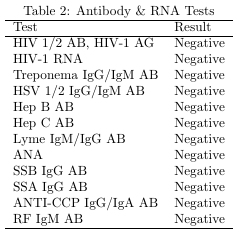
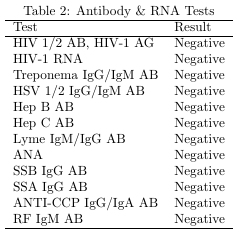
My primary suspicion has been an infectious disease, possibly HIV, but the tests so far don't paint a clear picture. First of all, HIV tests as shown in Table 2 have been negative. The CD4 percentage and CD4/CD8 ratio are both in the bottom 5-6% of the reference population which could indicate a progressive loss of CD4 cells. I don't have enough data yet to determine the trend. Generally, immunoglobulin levels would be raised so the low total IgM and low IgG subclasses don't necessarily fit that. Although, maybe there could be multiple independent conditions. I'm less confident in the HIV-2 test result as it only detects antibodies. If my antibody response is weakened from the IgG Subclass 1 deficiency, maybe it wouldn't be detected.
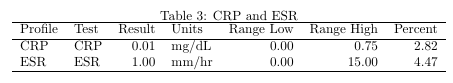
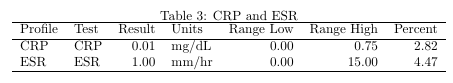
Another thing I might expect is inflammation markers to be somewhat elevated. However as shown in Table 3, ESR and CRP are both approaching the lower limits of the reference range.
Also, I recently attempted to have the Spectracell Micronutrient test performed and found out that it failed. Apparently my lymphocytes didn't sufficiently respond to mitogen stimulation. The lab said the blood was fine, no hemolysis, sufficient volume, and sufficient lymphocyte count. However, they did ask if I was taking any immunosuppressant medication or had a known deficiency. They have the following message on the website for the test:
***IMPORTANT NOTE: If a patient has leukemia, HIV/AIDS, Auto-Immune Condition or is known or suspected to have a low white blood cell count, please collect 3 CPT tubes of whole blood. A low white cell count can result in too few viable cells available for culture and testing***
I figured since all of my lymphocyte counts were within reference ranges (not by a lot in some cases though) that it would work without the extra blood, but I guess not. The lab did say that the test doesn't work for some people, but it sounded rare.
For reference, here are the symptoms currently impacting my quality of life:
- Persistent Fungal Infections (skin and nails)
- Chronic Dry Mouth
- Vision Problems (increased floaters, reduced acuity)
- Joint Stiffness & Cracking (especially knees and ankles)
- Muscle weakness (especially legs, loose kneecaps, sore tendons)
- Foot Pain (foot pad atrophy)
I have had a number of lab tests done which resulted in a couple results outside the reference range and a number of results approaching the limits. Table 1 shows all lab results that were in the bottom 10% of the reference range. The Percent column was calculated using the CDF assuming a normal distribution with a 95% reference interval. Therefore 2.5% represents the lower reference interval limit.
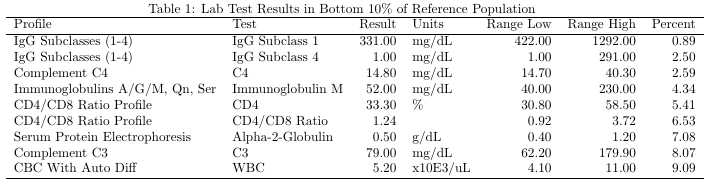
IgG Subclass 1 is below the reference interval and in the bottom 0.89% of the reference population. I recently discovered this deficiency and am not sure if it would affect antibody production and invalidate the results of previous antibody tests. I am concerned about the possibility though. As can be seen, a number of other immune system related markers are approaching the lower limits as well.
My primary suspicion has been an infectious disease, possibly HIV, but the tests so far don't paint a clear picture. First of all, HIV tests as shown in Table 2 have been negative. The CD4 percentage and CD4/CD8 ratio are both in the bottom 5-6% of the reference population which could indicate a progressive loss of CD4 cells. I don't have enough data yet to determine the trend. Generally, immunoglobulin levels would be raised so the low total IgM and low IgG subclasses don't necessarily fit that. Although, maybe there could be multiple independent conditions. I'm less confident in the HIV-2 test result as it only detects antibodies. If my antibody response is weakened from the IgG Subclass 1 deficiency, maybe it wouldn't be detected.
Another thing I might expect is inflammation markers to be somewhat elevated. However as shown in Table 3, ESR and CRP are both approaching the lower limits of the reference range.
Also, I recently attempted to have the Spectracell Micronutrient test performed and found out that it failed. Apparently my lymphocytes didn't sufficiently respond to mitogen stimulation. The lab said the blood was fine, no hemolysis, sufficient volume, and sufficient lymphocyte count. However, they did ask if I was taking any immunosuppressant medication or had a known deficiency. They have the following message on the website for the test:
***IMPORTANT NOTE: If a patient has leukemia, HIV/AIDS, Auto-Immune Condition or is known or suspected to have a low white blood cell count, please collect 3 CPT tubes of whole blood. A low white cell count can result in too few viable cells available for culture and testing***
I figured since all of my lymphocyte counts were within reference ranges (not by a lot in some cases though) that it would work without the extra blood, but I guess not. The lab did say that the test doesn't work for some people, but it sounded rare.
For reference, here are the symptoms currently impacting my quality of life:
- Persistent Fungal Infections (skin and nails)
- Chronic Dry Mouth
- Vision Problems (increased floaters, reduced acuity)
- Joint Stiffness & Cracking (especially knees and ankles)
- Muscle weakness (especially legs, loose kneecaps, sore tendons)
- Foot Pain (foot pad atrophy)
