Gut bugs misbehaving?
http://phoenixrising.me/archives/20926
The gut flora as a forgotten organ
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1500832/
Resistant starch
http://en.wikipedia.org/wiki/Resistant_starch
The Resistant Starch Challenge
http://forums.phoenixrising.me/inde...ge-is-it-the-key-weve-been-looking-for.26976/
http://www.aspirenaturalhealth.com/...e-puzzle-post-149-by-dr-tim-gerstmar-3262012/
http://www.naturopathydigest.com/archives/2006/jun/vasquez.php
Disclaimer
The information on this thread is not intended to be medical advice. The information is meant to inspire and motivate you to make your own decisions surrounding your health care and dietary needs. It is intended for educational and informational purposes only. You should not rely upon any information found on this thread to determine dietary changes, a medical diagnosis or course of treatment. Readers should perform their own research and make decisions in partnership with their own health care providers. Any statements or claims about the possible health benefits obtained from any foods or supplements mentioned on this thread have not been evaluated by the Food & Drug Administration and are not intended to diagnose, treat, cure or prevent any disease.
Contribution of dietary protein to sulfide production in the large intestine http://ajcn.nutrition.org/content/72/6/1488.full
Sulfate-reducing bacteria
http://en.wikipedia.org/wiki/Sulfate-reducing_bacteria
http://phoenixrising.me/archives/20926
The “Forgotten Organ”:
Gut Flora and Its Role in Immune Function
http://primaldocs.com/opinion/forgotten-organ-gut-flora-role-immune-function/
The main functions of the digestive system were once believed to include little beyond the breakdown of food into usable energy for the body and elimination of waste, the digestive tract is also home to 100 trillion microorganisms, known as the gut flora. The majority of these microorganisms are bacteria, with a small percentage consisting of fungi and protozoa. The functions of the gut flora are complex enough to resemble those of an organ, leading some researchers to refer to the gut flora as a “forgotten organ”. Indeed, the gut flora plays a number of roles so vital to the human body that if the gut were to be sterilized, long-term survival would be unlikely.
Types of Gut Flora
There are three main categories of microorganisms found in the gut:
1.) Essential Flora: This is the “friendly” bacteria that is found in the gut. In the healthy individual, essential flora dominates and controls other types of less desirable microorganisms. When functioning normally, this type of flora is responsible for conducting numerous roles that keep the body healthy.
2.) Opportunistic Flora: This group of microbes is found in the gut in limited numbers that are strictly controlled by the essential flora in the healthy individual. This type of flora is capable of causing disease if the essential flora becomes compromised and is unable to control the growth and numbers of opportunistic flora.
3.) Transitional Flora: These are various microorganisms that are introduced into the body through eating and drinking. When the essential flora is healthy and functioning normally, this type of flora will pass through the digestive track without causing harm. However, if the essential flora is damaged, this group of microbes can cause disease.
Roles of the Essential Gut Flora
Beyond controlling the population of opportunistic and transitional flora, essential gut flora plays an active role in the normal digestion and absorption of food by producing enzymes that aid in the process of breaking down proteins, carbohydrates, and fats. It also aids in the transportation of minerals, vitamins, water, and other nutrients through the gut wall into the bloodstream for use by the body. Certain types of essential flora are capable of manufacturing nutrients such as vitamins K2, B1, B2, B3 B6, B12, folic acid, pantothenic acid, and various amino acids. In addition to producing these nutrients to be used directly by the body, the essential flora provides nourishment to the cells of the intestinal wall that have primary responsibility for digesting and absorbing food. When the essential gut flora are compromised and not functioning normally, it is common for the individual to become malnourished and have multiple nutrient deficiencies and food intolerances.
Gut Flora and Immune Function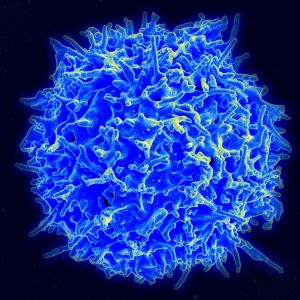
In the last decade or so, the importance of the gut flora to immune function, overall health, and disease has become an emerging area of focus. Although there is still much to be learned about the role of gut flora in immune function, it is becoming increasingly clear that disease (and health) really does begin in the gut! Studies have shown that the gut flora has a profound influence on the development and maturation of the immune system after birth (Bouskra et al., 2008; Macpherson & Harris, 2004). In addition, it has been estimated that approximately 80 -85% of the immune system is located in the gut.
In the healthy individual, the essential gut flora forms a bacterial layer that covers the entire digestive track. This bacterial layer acts as a physical barrier to protect against transitional flora , viruses, parasites, toxins, and undigested food particles. The gut flora produces acids that lower the pH of the gut wall and make it undesirable for microbes that cause disease. The essential flora also has the ability to neutralize many toxins and inactivate carcinogens (substances known to cause cancer). It also plays a direct role in suppressing the processes by which cancer cells are known to develop and grow.
The essential flora has a direct effect on important immune functions because it is responsible for stimulating the tissues of the lymph system that are located in the gut wall to produce lymphocytes, a type of white blood cell that fights infections. The lymphocytes then produce immunoglobulins, which are antibodies formed in response to contact with foreign substances (viruses, bacteria, fungi, etc). The immunoglobulins destroy and inactivate invading substances that enter the body through food and drink. The essential flora also has a direct impact on the function and/or production of other many other cells of the immune system. When the essential flora is damaged, immune function is affected not only in the gut, but systemically as well (throughout the entire body). Specific to autoimmune disease, essential gut flora plays an important role in the development of regulatory T cells, a critical component of the immune system. The types, number, and balance of regulatory T cells are directly influenced by the essential gut flora. The dysfunction of the regulation of different types of regulatory T cells (an imbalance in certain kinds of T cells) is responsible for the development of autoimmune disease.
A broader explanation of how the gut flora influences immune function is by understanding the balance between the two arms of the adaptive immune response, known as Th1 and Th2 immunity. In general, the role of Th1 immunity is to fight infections in the skin, mucous membranes, and cells. When the essential flora is damaged, the production and function of Th1 cells becomes impaired, allowing more invaders into the body. The body responds by overcompensating with a Th2 response. The overactive Th2 response then predisposes the individual to allergic-type reactions, chronic inflammation, and autoimmunity. Healthy essential gut flora is the key to keeping these arms of the adaptive immune system in balance, thus preventing disease.
The gut flora as a forgotten organ
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1500832/
Resistant starch
http://en.wikipedia.org/wiki/Resistant_starch
The Resistant Starch Challenge
http://forums.phoenixrising.me/inde...ge-is-it-the-key-weve-been-looking-for.26976/
Bacteria, especially Streptococcus, Enterococcus and Prevotella, can turn sulfur into hydrogen sulfide gas. Hydrogen sulfide gas smells like rotten eggs, is toxic to our nervous systems and our mitochondria.
So if we have a dysbiosis which contains a good deal of sulphate reducing bacteria, we have problems!
How do you know if you have this dysbiosis?
- Deficiency of sulfur which means
- Our nervous system doesn’t work properly - nerves can’t grow properly and neurotransmitters can’t be effectively broken down and removed meaning the levels of our neurotransmitters will be imbalanced, causing neurologic and behavioral issues.
- We can’t produce enough mucus to keep our guts healthy, meaning chronic issues with leaky gut.
- We can’t detoxify effectively - making people toxic (a whole host of problems) and chemically sensitive
- Excess hydrogen sulfide which is
- Toxic to our nervous system - double whammy when combined with sulfur deficiency
- Toxic to mitochondria - the energy producing parts of our cells. Leading to low energy in our cells and our bodies. Might lead to chronic fatigue like symptoms for some.
Here are some ways you might know you have a sulfur-reducing dysbiosis
- Intolerance to sulfur - there are several reasons people are intolerant to high sulfur containing foods, but this is one of them. Every time you eat foods with a lot of sulfur in them the bacteria reduce them to hydrogen sulfide and poison your body. So if you are intolerant to sulfur containing foods, it’s a good sign you may have this dysbiosis.
- Rotten egg flatulence - hydrogen sulfide smells like rotten eggs. If your flatulence (that’s the medical word for ‘farts’) are consistently foul, and especially if they smell like rotten eggs, that’s a good sign you have a good deal of sulfur-reducing bacteria.
- High sulfate reducing bacteria on a stool test - if you’ve had testing done that shows a lot of Streptococcus, Enterococcus and Prevotella it’s a sign you have this dysbiosis.
- Urinary testing - while I’ve never used this while doing some research for this article I found a small alternative lab that claims to test for hydrogen sulfide levels in the urine. If they are high, then that means you have a sulfur-reducing dysbiosis
What to do about it?
- Use antimicrobials - either prescription (antibiotics) if appropriate, or herbal to help kill the dysbiosis,
- Replace with probiotics - to help restore a healthy gut ecology and help prevent the return of dysbiosis.
- Consider green tea - an article about a recent study found, “At even lower concentrations — from 2.5 to 25 micrograms per milliliter — the polyphenols hindered the enzyme that catalyzes the formation of hydrogen sulfide, cutting its production by 30 percent. ” So green tea might be part of a protocol to reduce the production of hydrogen sulfide.
http://www.aspirenaturalhealth.com/...e-puzzle-post-149-by-dr-tim-gerstmar-3262012/
http://www.drmyhill.co.uk/wiki/Fermentation_in_the_gut_and_CFSTry to recreate the ideal environment for digestion of foods
One can test for a non-acid stomach by a simple saliva test - see Hypochlorhydria. There is no easy way to test for an alkali duodenum. Where there is hypochlorhydria, take additional acid with food (as ascorbic acid or betaine hydrochloride). The stomach normally takes 1-2 hours to empty; at this point take magnesium carbonate 1-2 grams, which neutralises stomach acid and assists digestion in the duodenum.
- Eat Diet of low fermentable substrate- it is sugar and refined carbohydrate which microbes most love to ferment. Bacteroides ferment vegetable fibre. The diet needs to be low glycaemic index (see Hypoglycaemia) and rich in raw or lightly cooked vegetables. However some people may also have to avoid vegetable fibre initially to starve out fermenting anaerobes in the upper gut. Indeed this is the basis of the GAPS diet developed by Dr Natasha Campbell McBride. Subsequently these foods can be reintroduced once the upper gut is healed. These foods contain a range of natural antimicrobials to inhibit bacterial overgrowth in the upper gut, together with many enzymes essential for their own digestion and fibre for fermentation in the large bowel by friendly bacteria into short chain fatty acids. This helps restore normal function. With fruit, some people will tolerate fructose because this is a monosaccharide and rapidy absorbed. Broadly speaking anaerobic bacteria ferment soluble fibre, aerobic bacteria ferment disaccharides, polysaccharides and starches (ripe fruit OK to eat because fructose is a monosaccharide) and yeast ferment mono-saccharides (ripe fruit not OK to eat!). The GAPS diet adresses fermentation by all three, the specific carbohydrate diet adresses fermetnation by aerobic bacteria. Anti candida diets adddress fermetnation by yeast. If in doubt suggest starting off with a protein fat diet for all the reasons given by Barry Groves in his lovely presentation. The only way to really find out is trial and error.
- Eat smaller meals - lesser amounts of foods are easier to deal with. Anyone who has eaten much too large a meal will recognise the symptoms of fermenting gut - fatigue, bloating, discomfort and, later, foul smelling wind!
- Sterilise the upper gut - the key here is to take something which kills bugs in the upper gut but does not upset bacteria in the lower gut. Bacteria and yeast are greedy for micronutrients, especially minerals. Indeed, this may explain why some patients worsen when they take micronutrients - these simply feed the upper gut flora so they ferment harder. Ways to tackle this:
Improve digestion
- Take high dose ascorbic acid or magnesium ascorbate between and during meals. The acid and the ascorbate both kill microbes. In the right dose they can sterilise the upper gut. If very high doses of vitamin C are taken it will spill over into the large bowel and cause diarrhoea - this is called taking vitamin C to bowel tolerance and is useful in getting rid of gut infections in a gastroenteritis.
- Take minerals through the skin by using transdermal micronutrients. This may explain why the tiny amounts of magnesium in injections is so effective!
- Plant tannins (eg viracin) chelate up minerals so they are not available to bugs. This may explain why tea drinking is so popular - the tannin in tea has the same effect. Also spicy foods kill microbes and may explain why the most popular British dish is now curry! Since gut fermentation is a common problem in people eating Western diets perhaps subconciously we have worked out that a good curry with a cup of tea makes us feel better!
- Broadly speaking it is yeast that ferment monosaccharides and disaccharides (sugar and fruit sugar), aerobic bacteria that ferment disaccharides and polysaccharides(grain and potato starches) and anaerobic bacteria that ferment soluble fibre.
Quick efficient digestion of food upstream means that there is less available to be fermented downstream. One may need:
- Acid supplements: Indeed, there may be a role for vitamin C as ascorbic acid. Ascorbic acid is acid and so improves digestion of protein. It is also toxic to all microbes including bacteria, yeast and viruses as well as being an important anti-oxidant - indeed the eventual receiver of most electrons from free radicals. Humans, guinea pigs and fruit bats are the only mammal species which cannot make their own vitamin C and we have to get it in food. Scaling up from other mammals we should be consuming 2-6 grams daily (a hundred fold more than the government RDA of 30mgs daily!). One could get the dose just right so that ascorbic acid with food sterilises the upper gut, but is absorbed and/or diluted so has a minimal effect on the lower gut. If one takes excessive vitamin C it will cause diarrhoea as too much gets into the lower gut, kills off the bugs there and empties the gut completely!
- Pancreatic enzymes see Pancreatic exocrine function. The need for these could be tested by doing a Comprehensive digestive stool analysis (CDSA). A dose would be 1-3 capsules of Polyzyme Forte (BioCare) with meals depending on the size of the meal. Be aware that many prescribable pancreatic enzymes contain toxic dimethicones or phthalates.
The body can use hydrogen sulfide in very low doses to help communicate and run things, in addition to nitric oxide and carbon monoxide – all ‘toxic’ gases. So it’s not that we want to get rid of all hydrogen sulfide, it’s that we want to get rid of overproduction which causes problems.
Antimicrobial treatments ("poison the microbes, not the patient"): Antimicrobial herbs can be used which directly kill or strongly inhibit the intestinal microbes. The most commonly used and well-documented botanicals in this regard are listed in the section below. Antimicrobial treatment frequently is continued for one to three months, and co-administration of drugs can be utilized when appropriate. Sometimes antimicrobial drugs are necessary, especially for acute and severe infections; often nutritional and botanical interventions are safer and more effective. Although these herbs generally are taken orally, some of them also can be applied topically (in a cream or lotion), and nasally (in a saline water lavage). Botanical medicines generally are used in combination, and lower doses of each can be used when in combination compared to the doses that are necessary when the herbs are used in isolation. When provided, dosage recommendations are intended for otherwise healthy adults; lower doses might be appropriate for children, the elderly and patients with renal or hepatic insufficiency.
Oregano oil in an emulsified, time-released tablet: Botanical oils that are not emulsified do not attain maximal dispersion in the gastrointestinal tract; products that are not time-released might be absorbed before reaching the colon in sufficient concentrations. Emulsified oil of oregano in a time-released tablet is proven effective in the eradication of harmful gastrointestinal microbes, including Blastocystis hominis, Entamoeba hartmanni, and Endolimax nana.18 An in vitro study19 and clinical experience support the use of emulsified oregano against Candida albicans. The common dose is 600 mg per day in divided doses (e.g., 150 mg four times per day) for at least six weeks.20
Berberine: Berberine is an alkaloid extracted from plants such as Berberis vulgaris and Hydrastis canadensis, and it shows effectiveness against Giardia, Candida, and Streptococcus, in addition to its direct anti-inflammatory and antidiarrheal actions. An oral dose of 400 mg per day is common for adults.21
Artemisia annua: Artemisinin has been used safely for centuries in Asia for the treatment of malaria,22,23 and it also has effectiveness against anaerobic bacteria, due to the pro-oxidative sesquiterpene endoperoxide. In a recent study treating patients with malaria, "The adult artemisinin dose was 500 mg; children aged < 15 years received 10 mg/kg per dose" and thus the dose for an 80-lb child would be 363 mg per day by these criteria.24 I commonly use artemisinin at 100 mg twice per day (with other antimicrobial botanicals such as berberine) in divided doses for adults with dysbiosis. One of the additional benefits of artemisinin is its systemic bioavailability.
St. John's Wort (Hypericum perforatum): Best known for its antidepressant action, hyperforin from Hypericum perforatum also shows impressive antibacterial action, particularly against gram-positive bacteria such as Staphylococcus aureus, Streptococcus pyogenes and Streptococcus agalactiae. According to in vitro studies, the lowest effective hyperforin concentration is 0.1 mcg/mL against Corynebacterium diphtheriae with increasing effectiveness against multiresistant Staphylococcus aureus at higher concentrations of 100 mcg/mL.25 Since oral dosing with hyperforin can result in serum levels of 500 nanogram /mL (equivalent to 0.5 microgram/mL) it's possible that high-dose hyperforin will have systemic antibacterial action. Regardless of its possible systemic antibacterial effectiveness, hyperforin clearly should have antibacterial action when applied "topically," such as when it's taken orally against gastric and upper intestinal colonization. Extracts from St. John's Wort hold particular promise against multidrug-resistant Staphylococcus aureus26 and perhaps Helicobacter pylori.27
Myrrh (Commiphora molmol): Myrrh is remarkably effective against parasitic infections.28 A recent clinical trial against schistosomiasis showed "The parasitological cure rate after three months was 97.4 percent and 96.2 percent for S. haematobium and S. mansoni cases with the marvelous clinical cure without any side-effects."29
Bismuth: Bismuth commonly is used in the empiric treatment of diarrhea (e.g., "Pepto-Bismol") and commonly is combined with other antimicrobial agents to reduce drug resistance and increase antibiotic effectiveness.30
Peppermint (Mentha piperita): Peppermint shows antimicrobial and antispasmodic actions and has demonstrated clinical effectiveness in patients with bacterial overgrowth of the small bowel.
Uva ursi: Uva ursi can be used against gastrointestinal pathogens on a limited basis per culture and sensitivity findings; its primary historical and modern use is as a urinary antiseptic that is effective only when the urine pH is alkaline. Components of uva ursi potentiate antibiotics.32 This herb has some ocular and neurologic toxicity and should be used with professional supervision for low-dose and/or short-term administration only.
Cranberry: Particularly effective for the prevention and adjunctive treatment of urinary tract infections, mostly by inhibiting adherence of E. coli to epithelial cells.
Thyme (Thymus vulgaris): Thyme extracts have direct antimicrobial actions and also potentiate the effectiveness of tetracycline against drug-resistant Staphylococcus aureus. Thyme also appears effective against Aeromonas hydrophila.
Clove (Syzygium species): Clove's eugenol has been shown in animal studies to have a potent antifungal effect.41
Anise: Although it has weak antibacterial action when used alone, anise does show in vitro activity against molds.42
Buchu/betulina: Buchu has a long history of use against urinary tract infections and systemic infections.43
Caprylic acid: Caprylic acid is a medium chain fatty acid that is commonly used in patients with dysbiosis, particularly that which has a fungal/yeast component. Beside empiric use, caprylic acid might be indicated by culture-sensitivity results provided with comprehensive parasitology.
Dill (Anethum graveolens): Dill shows activity against several types of mold and yeast.44
Brucea javanica: Extract from Brucea javanica fruit shows in vitro activity against Babesia gibsoni, Plasmodium falciparum,45 Entamoeba histolytica46 and Blastocystis hominis.47,48
Acacia catechu: Acacia catechu shows moderate in vitro activity against Salmonella typhi.
http://www.naturopathydigest.com/archives/2006/jun/vasquez.php
Disclaimer
The information on this thread is not intended to be medical advice. The information is meant to inspire and motivate you to make your own decisions surrounding your health care and dietary needs. It is intended for educational and informational purposes only. You should not rely upon any information found on this thread to determine dietary changes, a medical diagnosis or course of treatment. Readers should perform their own research and make decisions in partnership with their own health care providers. Any statements or claims about the possible health benefits obtained from any foods or supplements mentioned on this thread have not been evaluated by the Food & Drug Administration and are not intended to diagnose, treat, cure or prevent any disease.
Contribution of dietary protein to sulfide production in the large intestine http://ajcn.nutrition.org/content/72/6/1488.full
Sulfate-reducing bacteria
http://en.wikipedia.org/wiki/Sulfate-reducing_bacteria
Last edited by a moderator:
