Actually I'm tempted to go. If only to see what it's about.
There is something to be said for a first hand reconnaissance ......

Welcome to Phoenix Rising!
Created in 2008, Phoenix Rising is the largest and oldest forum dedicated to furthering the understanding of, and finding treatments for, complex chronic illnesses such as chronic fatigue syndrome (ME/CFS), fibromyalgia, long COVID, postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), and allied diseases.
To become a member, simply click the Register button at the top right.
Actually I'm tempted to go. If only to see what it's about.
I developed asthma from smoking in the early 80s. An Indian doctor at the hospital where I was working (I fancied him!) gave me an informal diagnosis and advice to give up smoking. I managed eventually to do the latter and it went away. It was pretty bad. Wheezing, struggling to breathe, using inhalers (when essential, as they caused the shakes and wakefulness).@ Irene - very true, and myself and my sister (asthmatic) are just old enough to have experienced that attitude from the medical profession and others. My sister was not taken seriously by the GP and denied treatment as a very young child and ended up in an oxygen tent - she was lucky. I'm interested to read your link later, thanks.
I do think things have thankfully changed now. No one is going to get away with claiming my asthma is somehow my mum's fault.
I also think that the system already in place in the UK using asthma nurses in GP surgeries (I don't know if it's universal)is likely to make spending resources on the approach in the cochrane report a nonstarter for asthma.
She's not GETSET Julie. That one started out very active, even before treatment.Like you also surprised that Julie is a real person.
Yes that's my fault, I was being silly. GETSET Julie is a fictional example dreamt up by the authors of that abominable leaflet - the woman in the video just happens to be called Julie too.She's not GETSET Julie. That one started out very active, even before treatment.
I would be tempted to use the phrase "physician, cure thyself" but first I would want evidence they actually have ME. If they just got a bit tired, claimed CFS, claimed it was therefore ME, and then got better after doing XYZ I would be justified in being sceptical.What would happen if one of them came down with ME...?
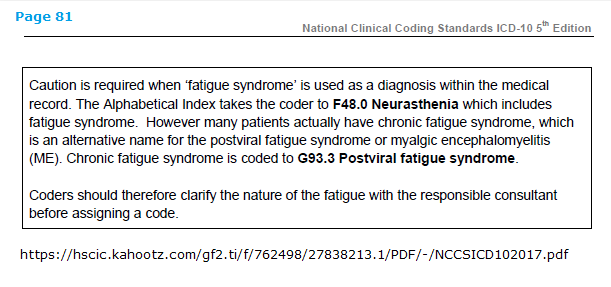
...The ICD-10 F45.0 coding for ME/CFS patients goes against the WHO classification but the Government appears to be insisting that it is still adhering to the WHO classification. It seems that they say one thing and do another.