Dx Revision Watch
Suzy Chapman Owner of Dx Revision Watch
- Messages
- 3,061
- Location
- UK
A custom TinyURL for this thread:
http://tinyurl.com/MUSnotforME
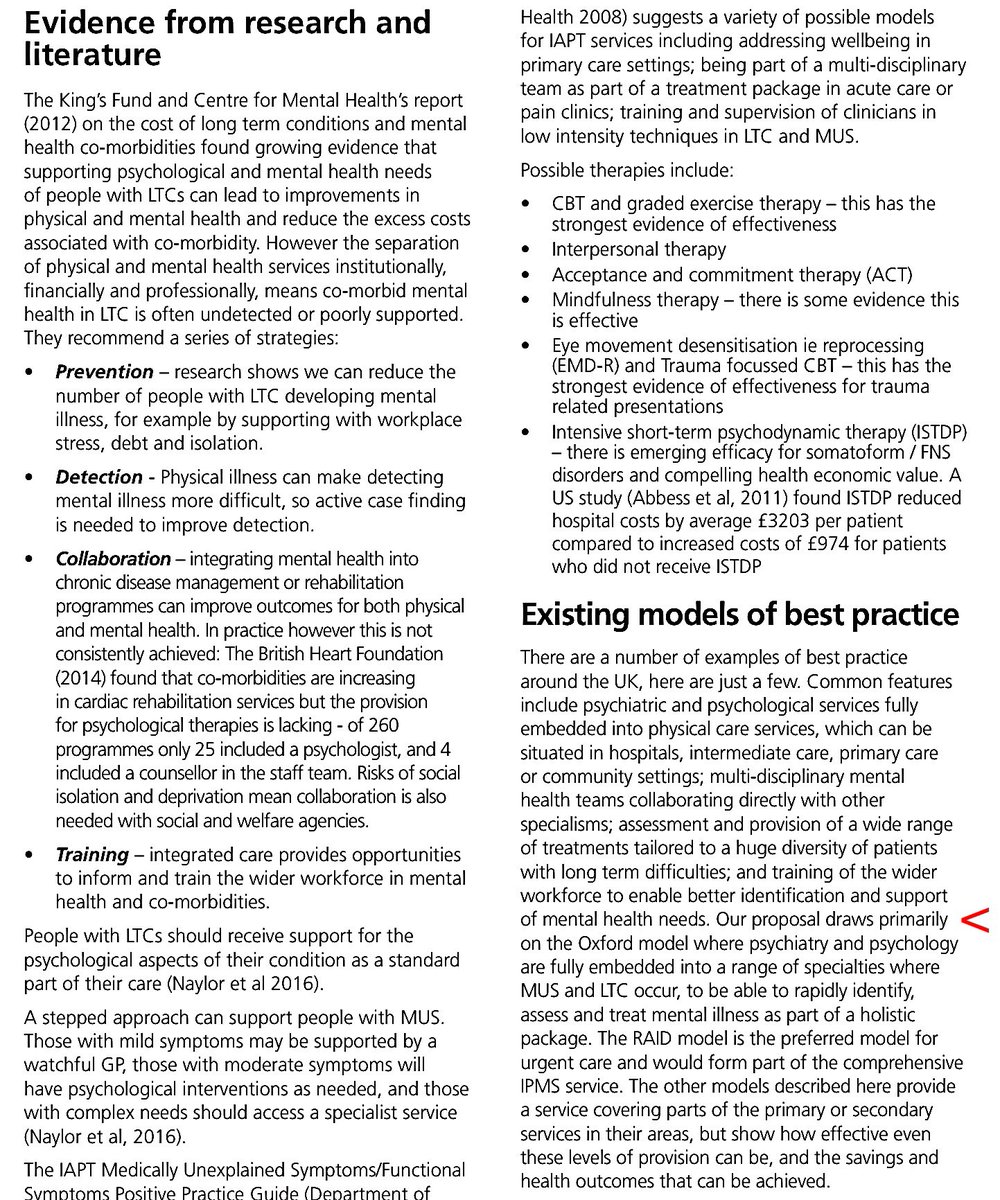
Services for Medically unexplained symptoms (MUS), Persistent physical symptoms (PPS) and integration into NHS primary care - what's happening across the UK?
I've been contributing to a thread in the Members Only forums in which I've posted material around commissioning of MUS and PPS services and their integration into primary care.
Several contributors suggested this material needs wider exposure and asked that I collate this material in a dedicated thread in the public forums.
Please add to this thread, now, or in the future:
http://tinyurl.com/MUSnotforME
Services for Medically unexplained symptoms (MUS), Persistent physical symptoms (PPS) and integration into NHS primary care - what's happening across the UK?
I've been contributing to a thread in the Members Only forums in which I've posted material around commissioning of MUS and PPS services and their integration into primary care.
Several contributors suggested this material needs wider exposure and asked that I collate this material in a dedicated thread in the public forums.
Please add to this thread, now, or in the future:
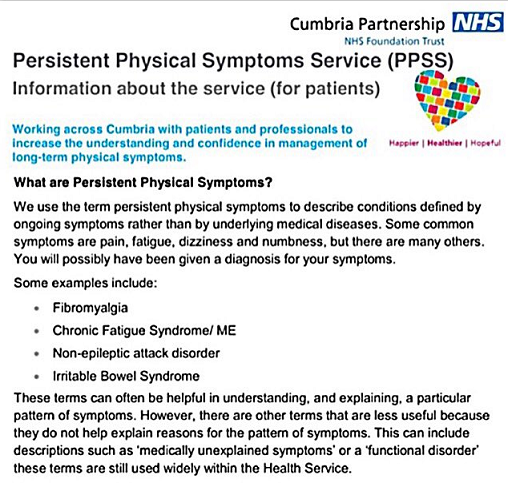
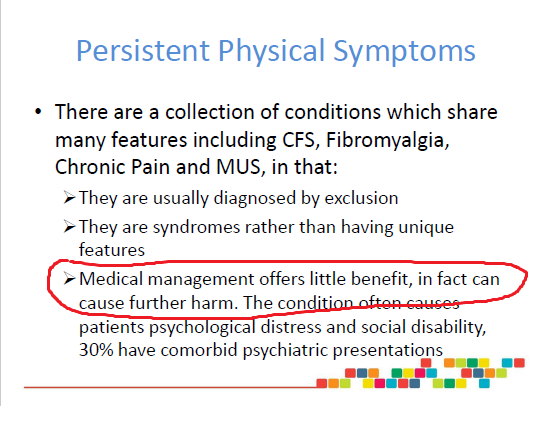
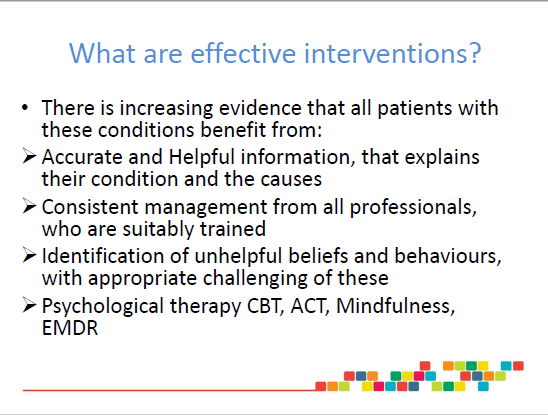
- if there are MUS or PPS services or GP managed MUS services or integrated IAPT services implemented or piloting in your own NHS Trust area;
- if you come across other examples of MUS or PPS services or GP managed MUS or IAPT services in other areas of the country;
- if you have been told by your GP that your ME, CFS, FM or IBS is now being managed as a MUS or PPS or under mental health disorders;
- if you have been referred to a MUS or PPS service or IAPT service;
- if your GP has recently expressed a change of views on the management of ME, CFS or has been pressuring you to accept a referral for CBT or for other psychological therapies.
- if your GP has recently reviewed your prescription med regime and is proposing to reduce or withdraw any medications that were specifically prescribed for managing your ME, CFS symptoms.
Last edited: