Old Bones
Senior Member
- Messages
- 808
I've coined the name "Mixed Orthostatic Intolerance Syndrome" to describe my current situation, and wonder if others experience the same.
Years ago, I was clinically diagnosed as having Neurally Mediated Hypotension. Over time, my adverse response to standing (feeling close to collapse) lessened. A few years ago I self-diagnosed POTS (based on HR and symptoms). I assumed POTS replaced the NMH, but now I'm not so sure.
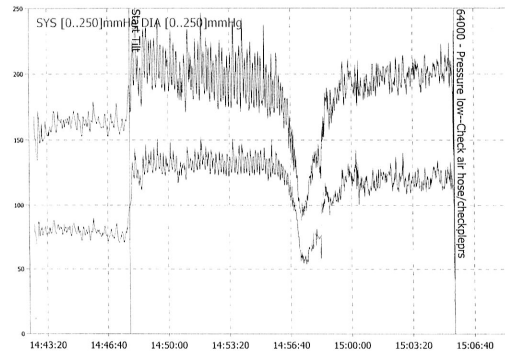
Yesterday, I decided to try the "poor man's tilt table test" at home. The difficulty, and results, were not what I expected. Here are my figures over 30 minutes of standing:
Resting: 103/60 HR 62
Immediately on standing: 102/75 HR - 101 bpm
Every five mins.: 102/85 - 107, 103/85 - 105, 124/71 - 108, 102/72 - 99, 110/80 - 102, 103/68 - 78
At about the 10-minute mark, I was starting to feel pretty shaky. At the 20-minute mark, I felt almost unbearably weak, and my breathing became irregular. At 25 minutes, I suddenly developed extreme abdominal cramps. At 30 minutes, I could no longer continue, the urgent need to lie down was so great. My face was deathly white, as though no blood was getting to my head.
Here's what surprised me . . . Yesterday, my blood pressure remained pretty stable, despite feeling even worse than I recall from years ago when my BP went as low as the 70/50 range while standing.
Does anyone know if a person can have Neurally Mediated Hypotension (based on symptoms alone) even if their BP isn't particularly low? What effect might POTS have on testing for NMH? Perhaps had I been able to stand a few minutes longer I would have seen the expected drop in BP. Is it possible to have both POTS and NMH?
Years ago, I was clinically diagnosed as having Neurally Mediated Hypotension. Over time, my adverse response to standing (feeling close to collapse) lessened. A few years ago I self-diagnosed POTS (based on HR and symptoms). I assumed POTS replaced the NMH, but now I'm not so sure.
Yesterday, I decided to try the "poor man's tilt table test" at home. The difficulty, and results, were not what I expected. Here are my figures over 30 minutes of standing:
Resting: 103/60 HR 62
Immediately on standing: 102/75 HR - 101 bpm
Every five mins.: 102/85 - 107, 103/85 - 105, 124/71 - 108, 102/72 - 99, 110/80 - 102, 103/68 - 78
At about the 10-minute mark, I was starting to feel pretty shaky. At the 20-minute mark, I felt almost unbearably weak, and my breathing became irregular. At 25 minutes, I suddenly developed extreme abdominal cramps. At 30 minutes, I could no longer continue, the urgent need to lie down was so great. My face was deathly white, as though no blood was getting to my head.
Here's what surprised me . . . Yesterday, my blood pressure remained pretty stable, despite feeling even worse than I recall from years ago when my BP went as low as the 70/50 range while standing.
Does anyone know if a person can have Neurally Mediated Hypotension (based on symptoms alone) even if their BP isn't particularly low? What effect might POTS have on testing for NMH? Perhaps had I been able to stand a few minutes longer I would have seen the expected drop in BP. Is it possible to have both POTS and NMH?