There are four basic types of hypoxia:
1. Hypoxic hypoxia occurs when there is a deficiency in oxygen exchange in the lungs.
Some causes include:
? Decreased partial pressure of oxygen available at altitude
? Conditions that block the exchange at the alveolar capillary level (e.g. pneumonia, pulmonary edema, asthma, drowning)
2. Anemic hypoxia occurs when the body cannot transport the available oxygen to the target tissues.
Causes include:
? Anemia from acute or chronic blood loss
? Carbon monoxide poisoning
? Medications such as aspirin, sulfonamides and nitrites
? Methemoglobinemia
? Sickle cell disease
3. Stagnant hypoxia occurs when there is insufficient blood flow.
Causes include:
? Heart failure
? Decreased circulating blood volume
? Excess vasodilatation
? Excess vasoconstriction
? Hyperventilation
4. Histotoxic hypoxia occurs when the bodys tissues are not able to use the oxygen that has been delivered to them.
Causes include:
? Hydrogen sulfide (mitochondrial toxin)
? Cyanide (mitochondrial toxin)
? Alcohol (mitochondrial toxin)
? Narcotics (mitochondrial toxin)
? Pesticides (mitochondrial toxin)
? Peroxynitrite (mitochondrial toxin)
? Antiretroviral drugs (mitochondrial toxin)
? Low CO2, hyperventilation (high oxygen affinity of hemoglobin)
? Carbon monoxide (high oxygen affinity of hemoglobin)
? Hypothermia (high oxygen affinity of hemoglobin)
? Alkalosis (high oxygen affinity of hemoglobin)
? Low phosphate (high oxygen affinity of hemoglobin)
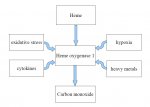
Most important causes of hypoxia in ME/CFS:
? Anemic hypoxia: Low red cell mass
? Stagnant hypoxia: Low blood volume, Excess vasoconstriction (high norepinephrine/endothelin/angiotensin)
? Histotoxic hypoxia :All mitochondrial toxins, High oxygen affinity of hemoglobin*
* Oxygen affinity of hemoglobin (p50) is calculated from venous blood gas values.
Excel program to calculate p50 from venous blood gas values:
http://www.medsci.org/v04p0232.htm