Ecoclimber
Senior Member
- Messages
- 1,011
Permission to Post by Prof. G
I found this research paper interesting as it is indicative of impairment in cerebral blood. There have been research studies on ME/CFS concerning cerbral blood flow reduction. All the elements of brain hypoxia, oxidative stress, brain inflammation are here: Eco
Is MS starving the brain?
Impaired Cerebrovascular Reactivity in Multiple Sclerosis
Olga Marshall, MS; Hanzhang Lu, PhD; Jean-Christophe Brisset, PhD; Feng Xu, PhD; Peiying Liu, PhD; Joseph Herbert, MD; Robert I. Grossman, MD; Yulin Ge, MD
JAMA Neurol. 2014;71(10):1275-1281. doi:10.1001/jamaneurol.2014.1668

IMPORTANCE
Cerebrovascular reactivity (CVR) is an inherent indicator of the dilatory capacity of cerebral arterioles for a vasomotor stimulus for maintaining a spontaneous and instant increase of cerebral blood flow (CBF) in response to neural activation. The integrity of this mechanism is essential to preserving healthy neurovascular coupling; however, to our knowledge, no studies have investigated whether there are CVR abnormalities in multiple sclerosis (MS).
OBJECTIVE
To use hypercapnic perfusion magnetic resonance imaging to assess CVR impairment in patients with MS.
DESIGN, SETTING, AND PARTICIPANTS
A total of 19 healthy volunteers and 19 patients with MS underwent perfusion magnetic resonance imaging based on pseudocontinuous arterial spin labeling to measure CBF at normocapnia (ie, breathing room air) and hypercapnia. The hypercapnia condition is achieved by breathing 5% carbon dioxide gas mixture, which is a potent vasodilator causing an increase of CBF.
MAIN OUTCOMES AND MEASURES
Cerebrovascular reactivity was calculated as the percent increase of normocapnic to hypercapnic CBF normalized by the change in end-tidal carbon dioxide, which was recorded during both conditions. Group analysis was performed for regional and global CVR comparison between patients and controls. Regression analysis was also performed between CVR values, lesion load, and brain atrophy measures in patients with MS.
RESULTS
A significant decrease of mean (SD) global gray matter CVR was found in patients with MS (3.56 [0.81]) compared with healthy controls (5.08 [1.56]; P = .001). Voxel-by-voxel analysis showed diffuse reduction of CVR in multiple regions of patients with MS. There was a significant negative correlation between gray matter CVR and lesion volume (R = 0.6, P = .004) and a significant positive correlation between global gray matter CVR and gray matter atrophy index (R = 0.5, P = .03).
CONCLUSIONS AND RELEVANCE
Our quantitative imaging findings suggest impairment in functional cerebrovascular pathophysiology, by measuring a diffuse decrease in CVR, which may be the underlying cause of neurodegeneration in MS.
This piece of research is a game-changer in my books; I don't think I quite appreciated how complex this disease is until I came across this article last night! Not only have we to contend with a frankly a confused immune system, but we now also have to think about strategies to combat brain hypoxia (the lack of oxygen) and ischaemic injury (lack of oxygen leading to areas of stroke) caused by the presence of vascular abnormalities observed in MS (see figure below).
The authors may be onto something here, and large scale brain hypoxia may be the penultimate factor/missing link in the spiraling trajectory towards brain atrophy in MS.
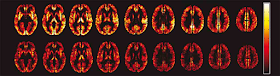
Figure: The mean gray matter cerebrovascular reactivity (CVR) maps of the control group (top) and multiple sclerosis group (bottom) show the diffuse decrease of CVR in the patients with multiple sclerosis. The color bar shows the range of CVR values (white=good CVR, black=poor CVR).
They postulate that abnormalities in CVR observed in MS may be the result of vascular (i.e. the vessel wall) habituation to nitric oxide (which results in vessel wall dilatation) produced during the chronic inflammatory process, ultimately leading to narrowing of blood vessels. But, I don't think this is the cause in entirety. This theory ignores the fact that the vessel wall (aka endothelium) also locally produces factors that regulate blood vessel tone, and the role of blood pressure, which is the largest regulator of perfusion to vital organs.
It is clear more work is needed in this area. And no CCSVI has no role here.
Neuro Doc Gnanapavan at 00:00
12 comments:
Matt PerryTuesday, February 24, 2015 12:19:00 am
Is this related to how statins work for MS?
Neuro Doc GnanapavanTuesday, February 24, 2015 8:49:00 am
Not quite, this is not caused by microvasular disease secondary to hypercholesterolaemia. But having said this, no one really knows how simvastatin works in MS either, this is another black hole.
Tuesday, February 24, 2015 1:19:00 am
If nothing else, this seems to correlate with Dr. Swank's observational data re patient longevity on an extreme low fat diet v a standard diet. Am I correct that this suggests that ms patients would have significantly worse response to high blood pressure and or high cholesterol?
Neuro Doc GnanapavanTuesday, February 24, 2015 8:52:00 am
High blood pressure will have an impact, as reduced cerebrovascular reactivity affects cerebral autoregulation (the way the brain controls its blood supply).
Matt PerryTuesday, February 24, 2015 9:12:00 am
Is this effect something that happens from the start, or progresses over time? I guess my question is whether it is independent of inflammation (ie it still happens/progresses even if you're NEDA on a dmd)?
Tuesday, February 24, 2015 12:16:00 pm
Is MS causes everything and anything?
It seems that random stuff, from oxidative stress to caesarean births, is potentially attributed to MS causation. The theories are mental, frankly.
Alison FisherTuesday, February 24, 2015 12:23:00 pm
It appears that hemodynamic dysfunction precedes the inflammatory process - this paper is interesting
http://www.ncbi.nlm.nih.gov/pubmed/25679526
Tuesday, February 24, 2015 4:11:00 pm
You may take glee in announcing that that 'CCSVI is not involved here' but at least this paper acknowledges the 150+ years of post mortem evidence of vascular abnormalities being the cause of MS plaque damage, and not perpetuating the lie that it is an autoimmune disease! Hypoxia is also an effect of CCSVI so there is a great deal to be learned from these studies. It is just a shame that collaboration between neurology and cerebrovascular medicine seems so far away while we live in a (pharmaceutical) drug culture.
Yulin Ge (one of the authors of the above paper) presented this paper at ISNVD last year concluding that 'there is CERTAINTY of VASCULAR INVOLVEMENT in MS'
http://www.isnvdconference.org/images/Presentations/Session_V/Sunday_-_845_am_-_Hemodynamic_-_Ge.pdf
MouseDoctor2Tuesday, February 24, 2015 4:31:00 pm
The vascular abnormalities would appear to be as a result of inflammatory lesions so perhaps the autoimmune hypothesis still has some legs? These findings are very interesting and shows how the cerebral vasculature could contribute to the cascade of pathological events after lesion formation so will be a new and interesting area to explore further.
Certainly there is vascular involvement but it ain't CCSVI.
Shirley RenshawTuesday, February 24, 2015 4:43:00 pm
OMG ... you are seeing something we have been screaming about since November 21, 2009. Will you neurologists be claiming this as your own find? I hope so ... so we can get on with the theory of CCSVI. MS is only the end result because CCSVI is ignored by so called MS experts.
MouseDoctor2Tuesday, February 24, 2015 4:51:00 pm
Shirley, this has nothing to do with CCSVI.
Tuesday, February 24, 2015 4:50:00 pm
Anything in this to indicate that Hyperbaric Oxygen Therapy might be beneficial after all? (I understand there is currently no evidence to back up this therapy.)
Research studies have shown that Hypebaric Oxygen Therapy are not effective for ME/CFS patients. The big question is what is causing the Cerebrovascular reactivity? Eco
Cerebral Circulation Time is Prolonged and Not Correlated with EDSS in Multiple Sclerosis Patients: A Study Using Digital Subtracted Angiography.
Monti L1, Donati D2, Menci E1, Cioni S1, Bellini M1, Grazzini I1, Leonini S1, Galluzzi P1, Severi S3, Burroni L4, Casasco A5, Morbidelli L6, Santarnecchi E7, Piu P2.
Author information
Abstract
Literature has suggested that changes in brain flow circulation occur in patients with multiple sclerosis. In this study, digital subtraction angiography (DSA) was used to measure the absolute CCT value in MS patients and to correlate its value to age at disease onset and duration, and to expand disability status scale (EDSS). DSA assessment was performed on eighty MS patients and on a control group of forty-four age-matched patients. CCT in MS and control groups was calculated by analyzing the angiographic images. Lesion and brain volumes were calculated in a representative group of MS patients. Statistical correlations among CCT and disease duration, age at disease onset, lesion load, brain volumes and EDSS were considered. A significant difference between CCT in MS patients (mean = 4.9s; sd = 1.27s) and control group (mean = 2.8s; sd = 0.51s) was demonstrated. No significant statistical correlation was found between CCT and the other parameters in all MS patients. Significantly increased CCT value in MS patients suggests the presence of microvascular dysfunctions, which do not depend on clinical and MRI findings. Hemodynamic changes may not be exclusively the result of a late chronic inflammatory process.
I will mention this research paper on ME/CFS that has some bearing on this topic
J Neurol Sci. 2011 Feb 15; 301(1-2): 9–11.
Published online 2010 Dec 16. doi: 10.1016/j.jns.2010.11.018
PMCID: PMC3139492
NIHMSID: NIHMS256234
Cerebral Blood Flow Is Reduced in Chronic Fatigue Syndrome As Assessed by Arterial Spin Labeling
Bharat Biswal,1 Pratap Kunwar,2 and Benjamin H Natelson2,3
Abstract
Background
Chronic fatigue syndrome is diagnosed by a set of clinical criteria and therefore is probably heterogeneous. Earlier reports tested the hypothesis that the syndrome had a neurological substrate by doing studies of cerebral blood flow (CBF) but with discrepant results. One possible reason for the discrepancy was that relative CBF was assessed. We found reduced CBF in an earlier study of absolute CBF using xenon-CT. The purpose of this study was to use a second method of assessing CBF and to look within the study group for heterogeneity of responses.
Method
Eleven CFS patients and 10 age matched healthy controls underwent neuro-imaging using arterial spin labeling to determine their regional and global absolute CBF. A template was constructed based on the control data, and individual patient montages were compared on a case by case basis to determine if differences in regions of interest occurred.
Results
The patients as a group had significantly lower global CBF than the controls. The reduction in CBF occurred across nearly every region assessed. Nine of the 11 patients showed these reductions compared to the average control data, while two patients showed actual increases relative to the controls.
Conclusion
The data extend our earlier observation that CFS patients as a group have broad decreases in CBF compared to healthy controls. However, as expected, the effect was not homogeneous in that 2 of the 11 patients studied showed actual increases in CBF relative to controls.
Keywords: fatigue, cerebral blood flow, heterogeneous, absolute, relative, syndrom
Last edited:
