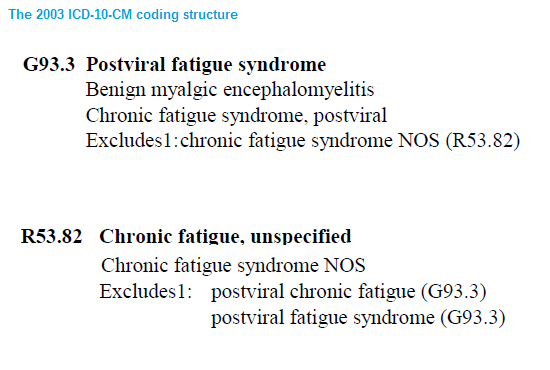
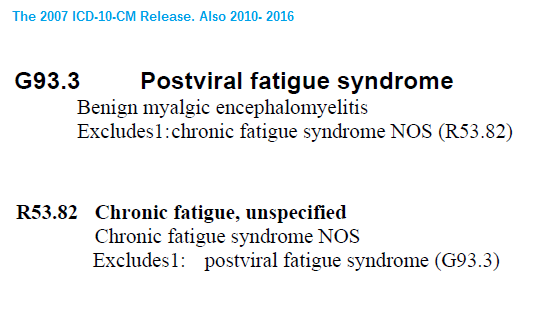
Note: It is too late to get SEID coded in ICD-10-CM, being adopted in the US on October 1. The IOM presented their report AFTER the deadline for filing for a change in ICD-10-CM's original version - and I believe they have also missed the deadline for filing for a change in ICD-10-CM when the first revision goes into effect, October 2016. Unless the Secretary of HHS personally intervenes (which I think unlikely), it will be a long time before SEID has a billable code. We in the US will continue to be stuck with ME at G93.3 and CFS at R53.82.
The deadline for submitting proposals for the March C & M meeting was January 16.
The deadline for the September C & M meeting was July 17.
So the deadline for the September meeting has already been reached.
However, even if a request for consideration of the addition of a new code had been submitted by July 17, and had been approved by NCHS Director, the partial code freeze on changes to the draft would have deferred the insertion of any new code.
The partial code freeze does not lift until 12 months following ICD-10-CM implementation.
http://www.cdc.gov/nchs/icd/icd9cm_maintenance.htm
Partial Freeze of Revisions to ICD-9-CM and ICD-10-CM/PCS
- The last regular, annual updates to both ICD-9-CM and ICD-10 code sets were made on October 1, 2011.
- On October 1, 2012, October 1, 2013, and October 1, 2014 there were only limited code updates to both the ICD-9-CM and ICD-10 code sets to capture new technologies and diseases as required by section 503(a) of Pub. L. 108-173.
- On October 1, 2015, there will be only limited code updates to ICD-10 code sets to capture new technologies and diagnoses as required by section 503(a) of Pub. L. 108-173. There will be no updates to ICD-9-CM, as it will no longer be used for reporting.
- On October 1, 2016 (one year after implementation of ICD-10), regular updates to ICD-10 will begin.
No new diagnosis codes were added for the 2015 Release or the 2016 Release. Requests for additions for insertion of new codes, for example, the APA's requests in September 2013 and March 2014 for insertion of a number of new DSM-5 diagnoses (including SSD), did not fulfill the criteria for capturing new diagnoses while a code freeze is in operation.
Most of the requests for insertion of new codes that have been submitted by any party since 2011, if approved, cannot be inserted until after the regular update and revision cycle has resumed. That includes the request for insertion of SSD under
F45.1 Undifferentiated somatoform disorder (if approved).
The Law
503(a) of Pub. L. 108-173 enabled the insertion of limited new diagnosis codes during a code freeze in order that codes to capture diseases like new strains of flu virus that have wide implications for public health could be rapidly inserted and would not have to wait until after an implemented code freeze had lifted.
The earliest that a new code that does not fulfill the conditions for consideration for insertion during a partial code freeze could be added (if approved by NCHS) is for on or after October 1, 2016. The 2016 Release was posted in June and contains no new diagnosis codes.
The deadline for the September 2015 C & M meeting has already been reached and the Tentative Agenda was posted, last week. The full Agenda isn't usually available until a day or two before Day One of a meeting, so a request for changes for consideration for
implementation after the code freeze lifts cannot be ruled out until the full Agenda for the September meeting has been posted.
The next meetings after the September 2015 meeting are scheduled for March and September 2016. Meetings are held in public and followed by public comment periods during which comments on requests presented at a meeting and/or suggestions for alternatives to what has been proposed via a meeting can be submitted by any stakeholder, via email. Occasionally a proposal will be resubmitted in revised form at a later meeting and the comment periods add several weeks to the process. Decisions on submissions aren't usually made public until the next Addendum and Release are issued.
The annual releases are posted around June, so the FY Release and Addendum for 2017 would be expected to be posted in mid 2016.
Small point, but the "CM" in ICD-10-CM stands for "Clinical Modification."
As Mary S has pointed out, ICD-10-CM is U.S. specific.
Responsibility for its update and revision is the purview of CMS/NCHS - not WHO, Geneva, though ICD-10-CM does incorporate some of the annual updates to the WHO's ICD-10.
The update and revision of the WHO's ICD-10 is the responsibility of an international body - the
WHO-FIC Update and Revision Committee which has a number of North American reps, including Donna Pickett.
ICD-10 is expected to continue to be revised for several more years but WHO has stated that it won't support revisions to ICD-10 indefinitely.
ICD-11 is now projected for presentation to WHA for approval/adoption in May 2018, but the ICD-11 package may not be ready for dissemination until later that year, or some point in 2019. Member States will need to evaluate the new edition and will transition from ICD-10 at their own pace - there is no mandated implementation date for adoption of ICD-11 by Member States.
It's not known when the UK NHSs would expect to transition to ICD-11. ICD-11 is still at the field testing stage and a great deal of work has still to be completed to produce a stable, usable product by 2018 that can be approved by WHA and that is also considered fit for purpose by the UN Statistical Commission and other stakeholder organizations.
ICD-11 is a considerably more complex package than ICD-10 was; it will be electronically based, has far more textual content, will be cross mapped to SNOMED-CT and will incorporate the various ICD Clinical Modifications as linearizations. It will require far more complex and costly preparations for adoption and implementation than the transition from ICD-9 to ICD-10.