Let me echo the thorough explanation by DX Revision watch. (FWIW, the presentation to CFSAC that had the new code for ICD-10-CM was made by Reeves AND by Donna Pickett from NCHS together.)
First and foremost - IF YOU DO NOT LIVE IN THE US, THIS HAS NOTHING TO DO WITH YOU (except as a precedent).
When you find "CM" at the end, it means "clinical manual' and it refers to the US adaptation. The US has been stuck on ICD-9-CM all this time - while everybody else long ago shifted to ICD-10. We are finally getting ICD-10-CM on October 1. I suspect it will be everything we feared Y2K would be, because all the doctors, clinics, and hospitals have to switch billing codes simultaneously, and my bet is that there will be a lot of computers that crash.
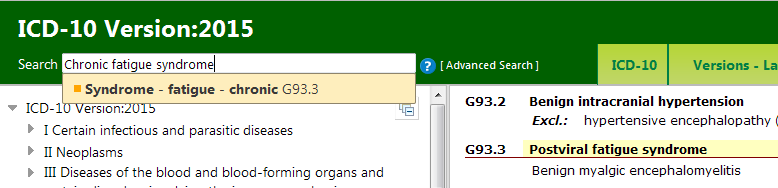
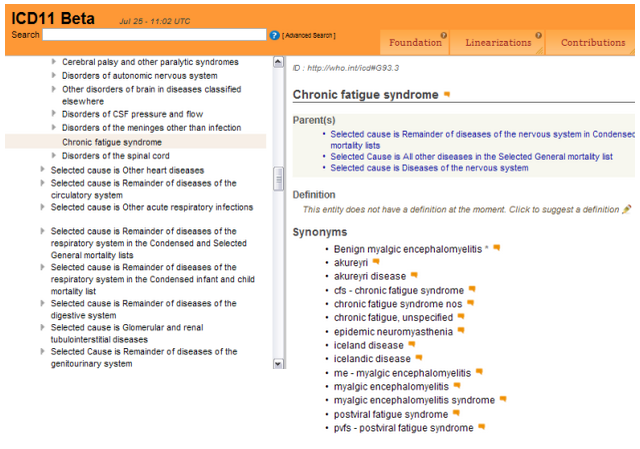
n ICD-10-CM, M.E. is coded at G93.3 in the chapter on neurological conditions, as it is in all the other nations' ICD-10 manuals.
BUT, in ICD-10-CM, CFS will be coded in R53.72, right next to chronic fatigue. TECHNICALLY, it says CFS (NOS). To understand why, a bit of history.
When the US adopted “chronic fatigue syndrome” in 1988, WHO was finalizing ICD-10, so they did not put it anywhere in ICD-9. As we all know, WHO later linked it to ME in G93.3 under neurology in ICD-10.
Since CFS was not in ICD-9, the US was free to put it wherever they wanted in ICD-9-CM. ME was at 323.9. But CFS was put at 780.71 in the back of the codes, under “vague signs and symptoms” and “malaise and fatigue”. (Which is, incidentally, where PVFS originally was placed in ICD-9.)
[NOTE: “CM” at the end of ICD-9 and ICD-10 means “clinical manual” and it refers to the US version of ICD-9 and ICD-10. Only a few nations do this formally - Canada, Australia, Germany are the others I am aware of. ICD-10-CA is Canada’s version (which brought us ME/CFS linked); ICD-10-AM is Australia’s; and ICD-10-GM is Germany’s, which has something that roughly translates as CFIDS - Chronic Fatigue and Immune Dysfunction Syndrome - coded equally with ME in G93.3. The rest of the world uses ICD-10 with perhaps minor adjustments.]
SO - for over 20 years ICD-9-CM, which has still been in force in the US (despite the rest of the world adopting ICD-10 years ago), has coded CFS apart from ME in the wastebasket diagnoses (what’s left after you diagnose other things) and, conspicuously, as a further qualified version of chronic fatigue. The US has done this on its own - NO OTHER NATION DOES THIS.
ICD-10-CM is the US version of ICD-10 and after all these years, the US is actually adopting it on October 1.
The agency charged with creating ICD-10-CM is NCHS, the National Center for Health Statistics, which is part of … CDC. And we all know what CDC thinks of this disease.
I first heard Donna Pickett at NCHS give a presentation to CFSAC about ICD-10-CM around 2004, and at the time they stated that CFS would go with ME in G93.3 in ICD-10-CM.
But the late Bill Reeves, who was then head of the CFS section at CDC, vociferously protested this (he said that he could only diagnose CFS as a subset of chronic fatigue … and anyway, there was no evidence of neurological abnormalities …)
SO, NCHS came back and gave a presentation where POSTVIRAL CFS would be coded at G93.3, but CFS (NOS) - (not otherwise specified) would go to R53.82, which is equivalent to the old ICD-9-CM code of 780.71. [Reeves said little but helped with the PowerPoint presentation.]
Then … somebody either at WHO or at CDC objected to “postviral CFS” because it was the same as postviral fatigue syndrome, PVFS, which was already in G93.3. So “postviral CFS” disappeared from G93.3 in ICD-10-CM (again, ONLY in the US version). But, so far, they have not gotten rid of the “NOS” after CFS in R3.82. Even though it isn’t otherwise specified anywhere.
To make this more complex, I don't know anybody in the US who diagnoses PVFS. I don't know anybody in the US with a diagnosis of PVFS. It's all CFS.
Okay. Understand that?
Then along comes the IOM committee, and gets all this totally wrong. We think that is because they used internet - in the US, if you do a quick search for codes in ICD-10, you will mostly get ICD-10-CM codes. All these billing firms are trying to get you to buy their program for converting ICD-9-CM codes to ICD-10-CM codes. But they don't often bother with -CM. They describe what i just explained as if it was in ICD-10, not just ICD-10-CM - which, of course, is wrong. So IOM formally stated the US was adopting ICD-10, and they said that CFS went in R53.82 in ICD-10. Which is wrong. WHO has NEVER coded CFS in R53.82. It may be in the index and not in the tabular version, but it is linked to G93.3.
Several of us - myself included - wrote to the chair of the IOM to warn her that this was factually wrong. so they “fixed” it - and STILL have it wrong. The published version states that in ICD-10, CFS is coded with ME in the chapter on neurology at G93.3. Okay. They also note that "fatigue syndrome" is coded at F48.0 with neurasthenia. also true.
But then they say the US is adopting ICD-10 on October 1, and that is NOT true. The US is adopting ICD-10-CM, our own version of ICD-10, and in our version, CFS is placed in R53.82 and further qualified as CFS (NOS).
However, I give them points for not only saying CFS was an inappropriate name (though I don’t find SEID much better) but also specifying that The Disease should not be coded with “chronic fatigue” (which is the R3.82 code) or “neurasthenia (F48.0, a particular favorite of Wessely and White for years). Under the circumstances, I’m not so sure that saying the US was adopting ICD-10 (and therefore G93.3 for CFS) on October 1 was a mistake. It may have been shrewd. Either way, however, it's inaccurate.
TECHNICALLY, it is against the rules of a signatory nation in WHO to change the CHAPTER in which a disease is placed in the ICD codes. So while it is okay to move M.E. around in the neurology codes, it is NOT okay to completely place a condition (CFS) in a different chapter entirely (R). So, TECHNICALLY, the US has violated the rules (or at least required an exemption) just for CFS! As near as we can figure, this is the only place that the US made such a change in ICD-10-CM. We're special. Isn't that nice?
Now, in the US, of course, we don’t hear anything about the WHO ICD codes except as they have been modified by the US - and they don’t usually tell us they were modified.
What Donna Pickett at NCHS (and Beth Unger at CDC) will tell you is that they didn’t want to “change” where CFS was coded, meaning they wanted to put it in ICD-10-CM in the equivalent to ICD-9-CM - a very self-centered approach, since it DOES represent a change from ICD-10 worldwide.
To repeat:
UNLESS YOU LIVE IN THE US, THIS DOES NOT AFFECT YOU AT ALL (except perhaps as a precedent).
And I, for one, am not at all sure whether I don’t prefer that ME and CFS remain separated - as long as ME does remain in ICD-10-CM. They used to play games with ME in ICD-9-CM where some years it was there and some years it wasn’t.
PS - My favorite incident (alluded to in the above post) was about ten years ago when Donna Pickett at NCHS came back to explain where CFS would go in ICD-10-CM, clearly after having had some discussions with Bill Reeves, and they put their powerpoint display unto a whiteboard that was just behind the chair’s seat. You could see CFS (postviral) in G93.3, but CFS (NOS) at R53.82 happened to fall off the bottom of the whiteboard and could only be seen by the spectators who looked around the board at the wall - it could not be seen at all by the committee members. Another person attending showed it to me - and not being particularly shy about these things, I stood up and said - “Wait! What’s that last line?” Bill Reeves glared at me and raised the projector so you could see R53.82. Hee hee.
As a side note for those in the US, diseases given the (NOS) add-on may not be covered by insurance … I have not checked this out, but several people have told me this is so.
Isn’t this fun? (It’s also why I think October 1, when across the US hospitals and doctors and clinics have to shift from ICD-9-CM coding to ICD-10-CM coding, is going to be what everybody thought Y2K would be, and it wasn’t. If your appendix is starting to act up, go to Canada … that sound in the background will be all the medical billing computers crashing...)