-

Welcome to Phoenix Rising!
Created in 2008, Phoenix Rising is the largest and oldest forum dedicated to furthering the understanding of, and finding treatments for, complex chronic illnesses such as chronic fatigue syndrome (ME/CFS), fibromyalgia, long COVID, postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), and allied diseases.
To become a member, simply click the Register button at the top right.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
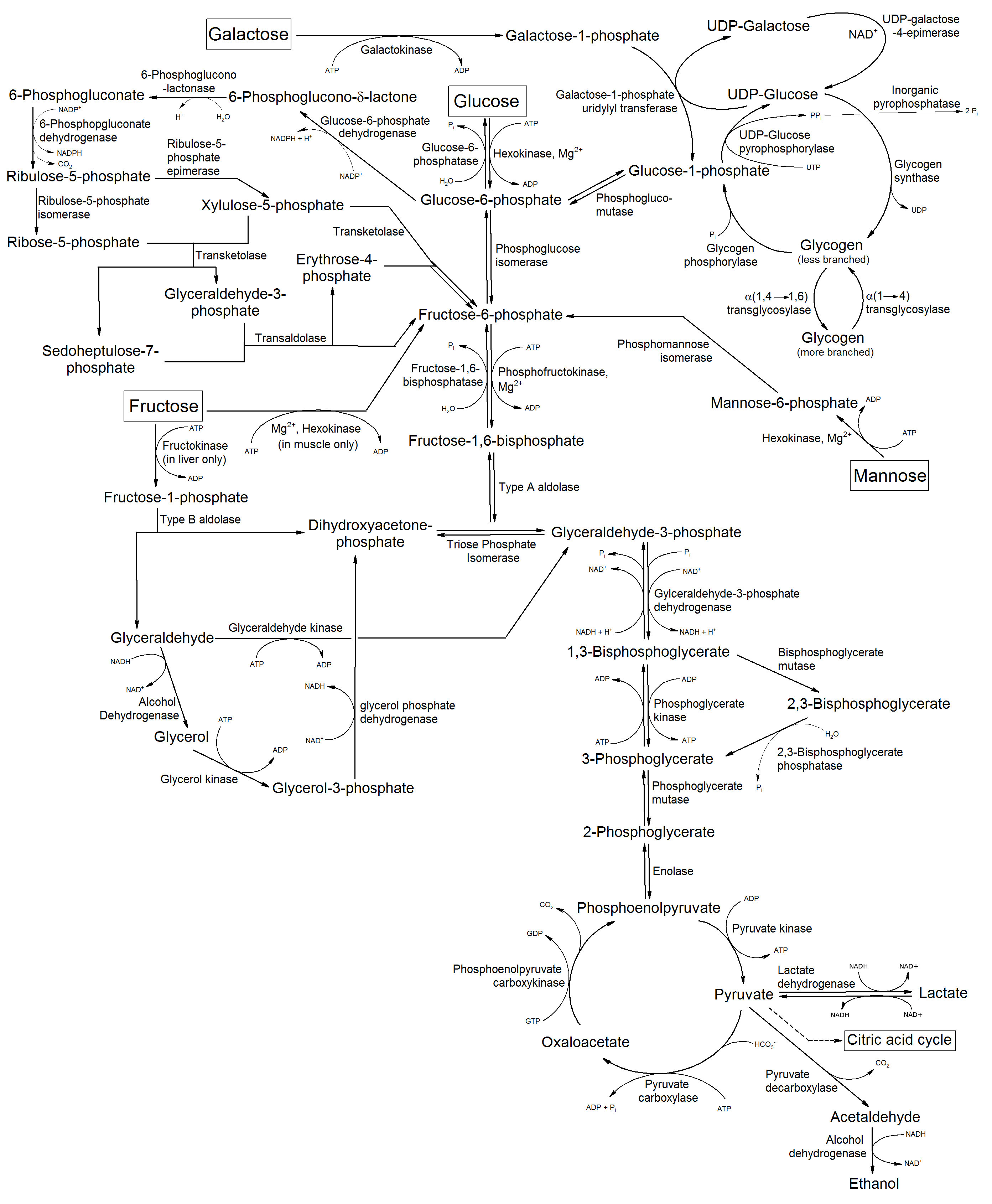
(Glycogenosis) The many roads to Glycogen Storage Depletion
- Thread starter Radio
- Start date
Carbohydrate-Deficient Glycoprotein Syndrome
http://en.wikipedia.org/wiki/Congenital_disorder_of_glycosylation
http://en.wikipedia.org/wiki/Congenital_disorder_of_glycosylation
Ribose Metabolism main co-factor is NAD+ / Niacinamide...
Several metabolic routes allow NAD+ synthesis from four different precursors (blue box). In the de novo pathway, NAD+ is synthesized from L-tryptophan, which is converted to quinolinic acid (not shown) and then to nicotinic acid mononucleotide (NaMN). An import pathway originates with nicotinic acid (Na), which is converted to NaMN (through the Preiss–Handler pathway), nicotinic acid adenine dinucleotide and then NAD+. A salvage pathway uses nicotinamide (Nam) to regenerate NAD+(Refs 1, 2). Na and Nam are collectively referred to as niacin, or vitamin B3. A fourth, recently discovered route incorporates nicotinamide riboside in the salvage pathway106. NAD+ and its phosphorylated relative NADP (not shown) are used as cofactors in several different redox reactions that are catalysed by NAD+ dehydrogenases (yellow box). These reactions are not accompanied by any net consumption of the nucleotides. Conversely, a net loss of NAD+ is associated with ADP-ribose-transfer reactions that take place during ADP-ribose cyclization (orange box), mono- or poly(ADP-ribosyl)ation and the deacetylation of proteins (green boxes). All these ADP-ribose-transfer reactions link NAD+ metabolism and the energy status of the cell to various aspects of cellular signalling for different cellular functions. Free ADP-ribose or derivative molecules can result from poly(ADP-ribose) degradation, which is catalysed by PARG isoforms and hydrolases (ARHs; ADP-ribosylarginine hydrolases), or from O-acetyl-ADP-ribose hydrolysis by Nudix O-acetyl-ADP-ribose hydrolase. These molecules might participate in the activation of TRPM2 channels (which are involved in calcium entry)107 and might react with proteins (resulting in glycation), which can lead to severe endothelial dysfunction, as in the case of diabetes-mellitus-associated atherosclerosis and other cardiovascular diseases.

NaDS, NAD+ synthase; NaMNAT, nicotinic acid mononucleotide adenylyltransferase; Nampt, nicotinamide phosphoribosyl transferase; NaPRTase, nicotinic acid phosphoribosyltranferase; NMNAT, nicotinamide mononucleotide adenylyltransferase; Nrk1, nicotinamide riboside kinase-1; PARG, poly(ADP-ribose) glycohydrolase; PARP, poly(ADP-ribose) polymerase.
Several metabolic routes allow NAD+ synthesis from four different precursors (blue box). In the de novo pathway, NAD+ is synthesized from L-tryptophan, which is converted to quinolinic acid (not shown) and then to nicotinic acid mononucleotide (NaMN). An import pathway originates with nicotinic acid (Na), which is converted to NaMN (through the Preiss–Handler pathway), nicotinic acid adenine dinucleotide and then NAD+. A salvage pathway uses nicotinamide (Nam) to regenerate NAD+(Refs 1, 2). Na and Nam are collectively referred to as niacin, or vitamin B3. A fourth, recently discovered route incorporates nicotinamide riboside in the salvage pathway106. NAD+ and its phosphorylated relative NADP (not shown) are used as cofactors in several different redox reactions that are catalysed by NAD+ dehydrogenases (yellow box). These reactions are not accompanied by any net consumption of the nucleotides. Conversely, a net loss of NAD+ is associated with ADP-ribose-transfer reactions that take place during ADP-ribose cyclization (orange box), mono- or poly(ADP-ribosyl)ation and the deacetylation of proteins (green boxes). All these ADP-ribose-transfer reactions link NAD+ metabolism and the energy status of the cell to various aspects of cellular signalling for different cellular functions. Free ADP-ribose or derivative molecules can result from poly(ADP-ribose) degradation, which is catalysed by PARG isoforms and hydrolases (ARHs; ADP-ribosylarginine hydrolases), or from O-acetyl-ADP-ribose hydrolysis by Nudix O-acetyl-ADP-ribose hydrolase. These molecules might participate in the activation of TRPM2 channels (which are involved in calcium entry)107 and might react with proteins (resulting in glycation), which can lead to severe endothelial dysfunction, as in the case of diabetes-mellitus-associated atherosclerosis and other cardiovascular diseases.

NaDS, NAD+ synthase; NaMNAT, nicotinic acid mononucleotide adenylyltransferase; Nampt, nicotinamide phosphoribosyl transferase; NaPRTase, nicotinic acid phosphoribosyltranferase; NMNAT, nicotinamide mononucleotide adenylyltransferase; Nrk1, nicotinamide riboside kinase-1; PARG, poly(ADP-ribose) glycohydrolase; PARP, poly(ADP-ribose) polymerase.
Rich Van Konynenburg
"I'm just wondering if anyone here who has ME/CFS has also been found to be positive for glucose-6-phosphate dehydrogenase deficiency (G6PDD). This is starting to be of some interest in autism, particularly in people of Middle Eastern or African descent, in which there is a greater prevalence of G6PDD, probably because malaria selected for people who had this genetic variation in the past.This is the most common genetic mutation in the human population. It causes red blood cells to be less able to recycle their glutathione, and can thus lead to early death of these cells. This is normally a disadvantage, but the benefit in malaria is that the malaria parasites inhabit the red blood cells and depend on the antioxidant system in the red blood cells for their survival. GDPDD would hamper control of oxidative stress,and that could help to kill the red cells in which the malaria parasites reside, and hence to knock out the parasites as well. Given that I believe that both ME/CFS and autism begin in most cases with depletion of the chemically reduced formof glutathione, and that red blood cells are normally net producers and exporters of glutathione, it would make sense from a theoretical point of view that having G6PDD would tend to increase the susceptibility to developing ME/CFS or autism."
Glucose-6-phosphate dehydrogenase deficiency
http://en.wikipedia.org/wiki/Glucose-6-phosphate_dehydrogenase_deficiency

"I'm just wondering if anyone here who has ME/CFS has also been found to be positive for glucose-6-phosphate dehydrogenase deficiency (G6PDD). This is starting to be of some interest in autism, particularly in people of Middle Eastern or African descent, in which there is a greater prevalence of G6PDD, probably because malaria selected for people who had this genetic variation in the past.This is the most common genetic mutation in the human population. It causes red blood cells to be less able to recycle their glutathione, and can thus lead to early death of these cells. This is normally a disadvantage, but the benefit in malaria is that the malaria parasites inhabit the red blood cells and depend on the antioxidant system in the red blood cells for their survival. GDPDD would hamper control of oxidative stress,and that could help to kill the red cells in which the malaria parasites reside, and hence to knock out the parasites as well. Given that I believe that both ME/CFS and autism begin in most cases with depletion of the chemically reduced formof glutathione, and that red blood cells are normally net producers and exporters of glutathione, it would make sense from a theoretical point of view that having G6PDD would tend to increase the susceptibility to developing ME/CFS or autism."
Glucose-6-phosphate dehydrogenase deficiency
http://en.wikipedia.org/wiki/Glucose-6-phosphate_dehydrogenase_deficiency

Last edited:
I was recently examined by sports medicine physician who used an ultrasound machine along with computer algorithm to indirectly measure quadricep glycogen levels. Ultrasound showed significantly depleted levels of muscle glycogen. I plan to have testing repeated after physical exertion. This test may be an objective way to quantify muscle fatigue in subset of CFS/ME patients.
An interesting question to consider is what causes glycogen depletion in CFS/ME patients. Some similarities might exist with ICU patients admitted for sepsis. Perhaps the link is the abnormal cytokines that puts skeletal muscles in a catabolic state.
The various glycogen storage diseases all have muscle pain and weakness as clinical manifestation.
What is the connection - viral trigger or chronic viral infection?
The various glycogen storage diseases all have muscle pain and weakness as clinical manifestation.
What is the connection - viral trigger or chronic viral infection?
Last edited:
pattismith
Senior Member
- Messages
- 3,937
Now you are back to where I was in 1997. My first model made a link between Tarui Disease (glycogen storage disease VII) and CFS. For a while I was called the phosphofructokinase guy. I postulated that phosphofructokinase was suppress in CFS by high concentrations of citric acid, and further postulated this might be due to a block at the Krebs Cycle enzyme aconitase. This disorder is accompanied by high uric acid. Several lines of research confirmed this until it was shown we have high phosphofructokinase activity.
soemthing more I have missed! So it is unlikely that EBV would block PFK, as suggested in this paper http://forums.phoenixrising.me/inde...igue-syndrome-using-peptide-microarray.52149/