How the analysis in this study works
This study, like several others trying to explain how CBT 'works' in CFS, uses a fearsome-sounding technique called Structural Equation Modelling, which I try to explain below:
Structural Equation Modelling (SEM)
SEM can prove theories wrong, or plausible, but not 'right'
This statistical approach is from the same family of techniques as the multivariate regression models routinely used in data analysis. What makes SEM different is that rather than try to analyse data and draw conclusions it looks through the other end of the telescope and asks: can this model explain the data? i.e. it starts with a theoretical model and sees if it holds up in experimental studies. SEM is set up in such a way that the model is 'falseifiable', that is it can be proven wrong by the data. But the model can't be proven 'right', only that it fits the data well and is a credible explanation. There may be several other credible explanations that would also fit the data.
So SEM can be a good way to compare 2 competing theories: one or both might be shown not to fit the data. Neither can be definitively proven right.
SEM can give insights into how a treatment works
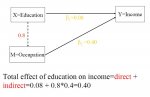
SEM is used in this paper to try to understand how CBT works - what
mediates the effect of the treatment. Mediation is probably best explained with an example: Income correlates with education, but income also correlates, unsurprisingly, with occupation too. However, occupation correlates strongly with education, as shown by the diagram below:
(from
presentation by Dr Peter Wang - slide 9)
So higher levels of education generally lead to higher incomes in later life, but the effect is
mediated by the effect of education on occupation. Better education leads to better jobs which leads to higher incomes.
Or watch a
short video that explains, with the aid of a tea towel, how SEM is used to probe mediation.
In this study the authors seek to show the effect of CBT was mediated by decreasing perceived problems with activity and a sense of control over fatigue. In other words, CBT works by changing perceived problems with activity and sense of control over fatigue - the mediators - which then produce the treatement effect of reduced fatigue.
However, to do this requires two things: first there must be a correlation between the mediators of activity problems perceived/sense of control and the outcome of reduced fatigue and second, that the mediators are changed first, then the outcome changes afterwards so there is a clear sequence of events. Without establishing this sequence of event no conclusions can be drawn over the direction of relationship. For instance, a reduction in fatigue may lead to a sense of control over fatigue, or both may be independently caused by CBT. Wheras in the example of education and income above, education takes place before the mediating factor of occupation giving much greater evidence of a causal relationship.