(click title to view blog properly)
Simon McGrath looks at theories that microglia, the brain's immune cells, could trigger and perpetuate the symptoms of ME/CFS and fibromyalgia.

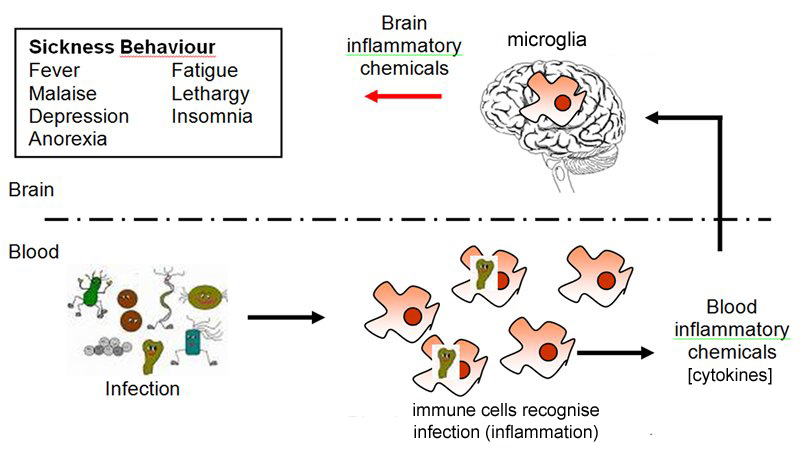
'Sickness Behaviour': the immune system releases cytokines in response to infection, which activates microglia in the brain and creates symptoms including fatigue, pain and cognitive problems.
Your dog can’t tell you when she's feeling sick, but even so, you know. She moves slowly, she doesn’t eat, she sleeps a lot, she curls up in a corner by herself. “Sickness behavior" is shared by all mammals, and in humans it’s been shown to include fatigue, cognitive problems, body aches and pains and disturbed sleep. These symptoms might sound very familiar to patients with ME/CFS and fibromyalgia, and several researchers recently have suggested that many core symptoms of these illnesses are the result of sickness behaviour biology gone wrong.
Understanding sickness behaviour first required uncovering some basics of the immune system. In the 1980s, scientists discovered a new molecule called Interleukin 1 that immune cells produce when they fight an infection. It was the first discovered example of a large class of messenger molecules called cytokines that help control the immune response.
Interleukin 1 was tried as a cancer treatment by boosting the immune system (with limited success), and patients reported that they experienced fatigue, pain and other problems that characterise sickness behaviour. This led scientists to the realization that sickness behaviour is driven by some cytokines.
Furthermore, they later discovered that these cytokines act on microglia, the brain’s immune cells, and it is ultimately the microglia that switch sickness response on or off. And the microglia may be where the problem with ME/CFS lies.Today’s blog post will describe the chain of events that lead to sickness response. Part two will describe how microglia could get stuck, triggering long-term sickness response and may perhaps be behind ME/CFS.
Sickness 'behaviour' - or response
The term “sickness behaviour” might sound like we’re dealing with psychological issues, but it’s actually describing an involuntary, physiological response to being sick.
The term was initially used to describe the behaviour of animals who rest and withdraw when sick, but it’s now used for the symptoms and underlying processes that drive that behaviour. In fact, Dr. Jarred Younger, a Stanford researcher who believes sickness behaviour may play a key role in the biology of Fibromyalgia and ME/CFS (see part two of the blog), would like to see the term sickness “behaviour” replaced by sickness “response.”
The term “sickness behaviour” might sound like we’re dealing with psychological issues, but it’s actually describing an involuntary, physiological response to being sick.
The term was initially used to describe the behaviour of animals who rest and withdraw when sick, but it’s now used for the symptoms and underlying processes that drive that behaviour. In fact, Dr. Jarred Younger, a Stanford researcher who believes sickness behaviour may play a key role in the biology of Fibromyalgia and ME/CFS (see part two of the blog), would like to see the term sickness “behaviour” replaced by sickness “response.”
Sickness Response | .ME/CFS (Fukuda)
Fatigue | Fatigue
Cognitive problems | Cognitive problems
Disturbed sleep | Disturbed sleep
Headaches | Headaches
Body aches & pains | Muscle & joint pain
Depressed mood | Post-exertional malaise
Pain hypersensitivity | Pain hypersensitivity (FM)
Social isolation | Sore throats
Anhedonia | tender cervical nodes
Post-exertional malaise is notably missing from sickness response, but the big overlap suggests that sickness response could be playing a substantial role in ME/CFS.
Fatigue | Fatigue
Cognitive problems | Cognitive problems
Disturbed sleep | Disturbed sleep
Headaches | Headaches
Body aches & pains | Muscle & joint pain
Depressed mood | Post-exertional malaise
Pain hypersensitivity | Pain hypersensitivity (FM)
Social isolation | Sore throats
Anhedonia | tender cervical nodes
Post-exertional malaise is notably missing from sickness response, but the big overlap suggests that sickness response could be playing a substantial role in ME/CFS.
The chain reaction that creates sickness response
From an evolutionary perspective, sickness response in response to infection is very useful. It forces us to be still, reserving energy for healing, and causes us to retreat where we’ll be safe from predators.
But it’s meant to be a short-term response of a week or so and if it lasts and lasts, that’s not so useful. If that happens, some part of the chain reaction that leads to sickness response has broken.
Infection almost always occurs in the body rather than the brain itself, because the brain protects itself from infection with a highly selective barrier that bacteria and viruses have a very hard time penetrating.
The blood-brain barrier also keeps out immune cells, though, so when the immune system detects infection in the body, it has only a couple of ways of letting the brain know about it. It releases cytokines that regulate immune response. These are able to pass through some parts of the blood brain barrier, but they can also communicate with the brain by stimulating the vagus nerve in the body, which in turn secretes cytokines into the brain.
The next step in the chain is that the cytokines activate the brain’s own immune cells, the microglia.
Microglia: powerhouse of immune response in the brain
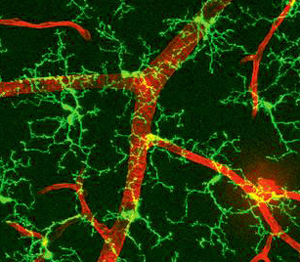
Because immune cells like B-cells, T-cells and Natural Killer cells can’t cross the blood-brain barrier, the brain largely relies on its own small, highly adaptable cells called microglia for immune protection. In their 'resting' state, microglia have cell bodies with many long fingers extending from a central cell body (see photo).
These cells are actually on patrol, extending and retracting fingers to 'scan' their territory by touch, lingering at nerve synapses in particular to check their health.
Such patrolling microglia scan their territories every few hours, their bodies remaining in the same place while their scanning fingers are almost a blur by the standards of the brain.
But that’s the quiet life for microglia. Once cytokines or other factors alert microglia to injury or infection, they shift into their activated form, zipping through the brain to where they are needed (see 20" video).
Once there, they spew out chemicals that set up the brain and body for recovery and, most importantly for ME/CFS (and fibromyalgia), that trigger sickness response: for example, neurones involved in perceiving fatigue fire more often.
So now we have the full chain of reactions that leads to sickness response:
Infection -> cytokines elevated in blood -> cytokines elevated in brain -> microglia activated -> microglia produce more cytokines -> sickness response
Simple! Thanks for your patience in sticking with all the biology - here's a summary in picture form:
How infection leads to sickness response, via cytokines and microglia.
(Image courtesy of Southampton University, labelling tweaked slightly for clarity.)
Part one of this blog has looked at how the body responds to infection with sickness response, via a chain of events including cytokines and microglia.
Part two will describe new theories about how the microglia could misfire, triggering sickness response for far longer than is intended and even leading to ME/CFS and fibromyalgia. Coming soon!
Simon McGrath tweets on ME/CFS research:
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
Read the Original Blog Post
Last edited: