And
this one.
Systemic Intracellular Bacterial Infections (Mycoplasma, Chlamydia, Borrelia species) in Neurodegenerative (Multiple Sclerosis, Amyotrophic Lateral Sclerosis, Alzheimer's) and Behavioral (Autistic Spectrum Disorders) Diseasesby Prof. Garth L. Nicolson
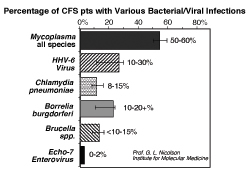
"Using the blood of 100 CFS/ME patients and forensic polymerase chain reaction, we found that a majority of patients show evidence of multiple, systemic bacterial and viral infections (Odds Ratio = 18.0, 95% CL 8.5-37.9, P< 0.001) that could play an important role in CFS/ME morbidity.11,79 CFS/ME patients had a high prevalence of one of four Mycoplasma species (Odds Ratio = 13.8, 95% CL 5.8-32.9, P<0.001) and often showed evidence of co-infections with different Mycoplasma species, Chlamydia pneumoniae (Odds Ratio = 8.6, 95% CL 1.0-71.1, P<0.01), and/or active HHV-6 (Odds Ratio = 4.5, 95% CL 2.0-10.2, P<0.001). We found that eight percent of the CFS patients showed evidence of C. pneumoniae and 31% of active HHV-6 infections.11,79 In a separate study, we found that a sizable percentage of CFS/ME patients were infected with Borrelia burgdorferi, and therefore, they were also Lyme disease patients.80"