View the Post on the Blog
The second in a new series of ‘In Brief’ articles, where Andrew Gladman provides a helpful insight into the science behind fairly common topics, exploring how they relate to ME/CFS. This time he discusses the adrenal glands and why they can be such a talking point ...

Diagram showing the location of the adrenal glands, above the kidneys
While the frequent topics of conversation relating to ME/CFS appear to now be infectious agents, autoimmunity and often a dysfunctional nervous system, many patients and researchers still turn their attention to problems within the endocrine system, namely the adrenal gland.
As the gland within the body centred around stress responses, it is initially quite a logical place to look for problems. There can be no denying that patients suffering with diseases of the adrenal glands certainly do share many symptoms and complaints of those afflicted with ME/CFS.
There is then good reason to query where the adrenal glands may relate to ME/CFS. While the initial reason for querying this may seem simple, the answers raise interesting questions for the potential pathophysiology and reasons for the symptomology of ME/CFS.
What are the Adrenal Glands?
The adrenal gland is one of the body's most vital endocrine glands. The adrenals are glands which secrete their hormone directly into the bloodstream, often as a result of the glands being innervated with blood vessels. Sitting above each kidney, these glands' primary function is releasing the hormones and chemicals which in turn stimulate a stress response, often known as a fight or flight reaction.
However the adrenal glands do carry out numerous other functions.
The stress response is initiated through the production and release of corticosteriods, such as cortistol, and a larger group of chemicals known as catecholamines of which adrenaline (epinephrine) and noradrenaline fall under.

Diagram showing the division between the adrenal medulla and cortex, along with the chemicals produced by each
The adrenal gland is composed of numerous layers although it is often discussed simply as being split into two main regions, the medulla and the cortex.
The medulla is the centre of the gland and the cortex is the outermost layers. The medulla is responsible for the production of adrenaline and noradrenaline. It achieves this through complex innervation with neurons of the sympathetic nervous system which stimulate the adrenal medulla in times of acute stress, increasing the rate of synthesis and release of these chemicals.
The cortex, on the other hand, is tasked with the production of corticosteroids, including cortisol and aldosterone, along with androgen hormones (the male sex hormones). The cortex is further sub-divided into three separate layers differentiated by which of the discussed chemicals is being produced by the specialised cells in that region, although the specifics of this sub-division are very rarely discussed.
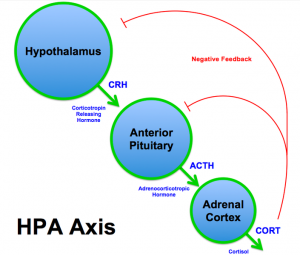
The HPA axis
Given the importance of the adrenal gland in producing these vital chemicals, there has evolved a complex set of interactions between other endocrine glands, the adrenal gland and the brain to help regulate one another through a process known as negative feedback.
This set of interactions occurs between the hypothalamus (a region at the centre of the brain), the pituitary gland (a small gland located at the base of the brain) and the adrenal gland. This set of interactions between these three areas is known commonly as the hypothalamic-pituitary-adrenal axis, often abbreviated to HPA axis.
It is this HPA axis that is frequently discussed in relation to ME/CFS.
Given the wide range of chemical messengers produced by the adrenal gland through the complex interactions it shares within the HPA axis, it is clear that the gland has far-reaching consequences within the homeostasis of the body.
These include playing roles in helping to control and regulate body temperature, digestion, immune system responses, mood sexuality and energy usage, along with the adrenal's primary function of controlling the physiological reaction to stress, trauma and injury.
It is clear to see why any dysfunction in either the adrenal gland alone or in the HPA axis as a whole could potentially cause a plethora of problems and symptoms. Dysfunction in the HPA axis is well known to be involved in a wide variety of psychological illnesses and is now being understood to play quite a large role in many physiological conditions too -- understandably, given the stress that disease itself causes.
Why are the Adrenal Glands important in ME?
For many years now studies have indicated finding abnormalities in HPA axis function within the ME/CFS cohort. These abnormalities are often described in the literature to include mild hypocortisolism, heightened negative feedback, and blunted HPA axis responsiveness.
Fundamentally, this means that in those patients observed, cortisol levels are persistently lower than is to be expected. This appears to be traced back to the hypothalamus and pituitary gland becoming somewhat unable to appropriately detect or respond to the low cortisol levels.
Many studies have not just identified this as a fairly consistent finding in ME/CFS but have furthermore observed a correlation between this dysfunction and symptom severity. It is of note however that some studies dispute this finding.
This dysfunction in the HPA axis has been used somewhat deviously by some groups to verify the effectiveness of talking-based therapies such as cognitive behavioral therapy (CBT).
This is in part due to the effectiveness these therapies can appear to have in conditions such as anxiety disorders in which HPA axis dysfunction has also been proven to play a somewhat central role. However such a line of thought, while helpful in many diseases where HPA axis appears to be a disease mediator, is unlikely to be helpful in a disease where the HPA axis does not yet appear to be central.
While there are a large number of studies confirming their independent findings of HPA axis dysfunction, few make the leap to develop a hypothesis for this being the central disease mechanism. This is likely a result of the multitude of other research indicating a deeper physiological defect in ME/CFS of which HPA axis may simply be an unfortunate by-product.
One interesting study that bears thought as to HPA axis dysfunction developing as a secondary condition is a somewhat unrelated study by Dunn et al. This study focuses upon how cytokines can in turn activate the HPA axis, initiating a stress response. Cytokines are a rapidly emerging line of study in ME/CFS and we recently produced an article exploring why they are gaining increased exposure in the ME/CFS research field.
It's an interesting notion that cytokines can directly influence the functioning of the HPA axis. When we consider the emerging results of researchers such as Prof. Lipkin outlining significant cytokine abnormalities in ME/CFS, perhaps we have a logical line of reasoning as to why the HPA axis appears somewhat blunted.
If the observed cytokine abnormalities prove repeatable and appear chronic, then it stands to reason that the HPA axis is under significant strain for a prolonged period of time. This could account for lower cortisol levels as time progresses, alongside a blunting of the HPA axis response when challenged with a stressor.
This hypothesis would also be supported by the HPA axis dysfunction seen in other chronic conditions with significant cytokine disturbance, such as lupus.
Overall, while problems with the adrenal glands and HPA axis function don't yet appear to be a sole causative agent for ME/CFS, they do provide an interesting explanation for certain symptoms of ME/CFS from which patients suffer. As time progresses, and through the thorough research done every day, we learn more and more about the complex interconnections between different organs and systems such as the HPA axis.
The connections between these systems, while seemingly unrelated to many diseases, appear to play quite a substantial role in the symptomolgy of ME/CFS, perhaps tying together with increasing evidence of autonomic dysfunction within ME/CFS.
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.

View the Post on the Blog
The second in a new series of ‘In Brief’ articles, where Andrew Gladman provides a helpful insight into the science behind fairly common topics, exploring how they relate to ME/CFS. This time he discusses the adrenal glands and why they can be such a talking point ...

Diagram showing the location of the adrenal glands, above the kidneys
While the frequent topics of conversation relating to ME/CFS appear to now be infectious agents, autoimmunity and often a dysfunctional nervous system, many patients and researchers still turn their attention to problems within the endocrine system, namely the adrenal gland.
As the gland within the body centred around stress responses, it is initially quite a logical place to look for problems. There can be no denying that patients suffering with diseases of the adrenal glands certainly do share many symptoms and complaints of those afflicted with ME/CFS.
There is then good reason to query where the adrenal glands may relate to ME/CFS. While the initial reason for querying this may seem simple, the answers raise interesting questions for the potential pathophysiology and reasons for the symptomology of ME/CFS.
What are the Adrenal Glands?
The adrenal gland is one of the body's most vital endocrine glands. The adrenals are glands which secrete their hormone directly into the bloodstream, often as a result of the glands being innervated with blood vessels. Sitting above each kidney, these glands' primary function is releasing the hormones and chemicals which in turn stimulate a stress response, often known as a fight or flight reaction.
However the adrenal glands do carry out numerous other functions.
The stress response is initiated through the production and release of corticosteriods, such as cortistol, and a larger group of chemicals known as catecholamines of which adrenaline (epinephrine) and noradrenaline fall under.

Diagram showing the division between the adrenal medulla and cortex, along with the chemicals produced by each
The adrenal gland is composed of numerous layers although it is often discussed simply as being split into two main regions, the medulla and the cortex.
The medulla is the centre of the gland and the cortex is the outermost layers. The medulla is responsible for the production of adrenaline and noradrenaline. It achieves this through complex innervation with neurons of the sympathetic nervous system which stimulate the adrenal medulla in times of acute stress, increasing the rate of synthesis and release of these chemicals.
The cortex, on the other hand, is tasked with the production of corticosteroids, including cortisol and aldosterone, along with androgen hormones (the male sex hormones). The cortex is further sub-divided into three separate layers differentiated by which of the discussed chemicals is being produced by the specialised cells in that region, although the specifics of this sub-division are very rarely discussed.
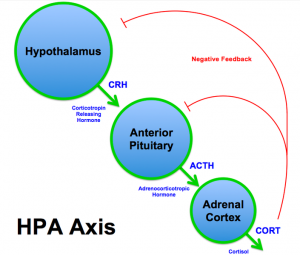
The HPA axis
Given the importance of the adrenal gland in producing these vital chemicals, there has evolved a complex set of interactions between other endocrine glands, the adrenal gland and the brain to help regulate one another through a process known as negative feedback.
This set of interactions occurs between the hypothalamus (a region at the centre of the brain), the pituitary gland (a small gland located at the base of the brain) and the adrenal gland. This set of interactions between these three areas is known commonly as the hypothalamic-pituitary-adrenal axis, often abbreviated to HPA axis.
It is this HPA axis that is frequently discussed in relation to ME/CFS.
Given the wide range of chemical messengers produced by the adrenal gland through the complex interactions it shares within the HPA axis, it is clear that the gland has far-reaching consequences within the homeostasis of the body.
These include playing roles in helping to control and regulate body temperature, digestion, immune system responses, mood sexuality and energy usage, along with the adrenal's primary function of controlling the physiological reaction to stress, trauma and injury.
It is clear to see why any dysfunction in either the adrenal gland alone or in the HPA axis as a whole could potentially cause a plethora of problems and symptoms. Dysfunction in the HPA axis is well known to be involved in a wide variety of psychological illnesses and is now being understood to play quite a large role in many physiological conditions too -- understandably, given the stress that disease itself causes.
Why are the Adrenal Glands important in ME?
For many years now studies have indicated finding abnormalities in HPA axis function within the ME/CFS cohort. These abnormalities are often described in the literature to include mild hypocortisolism, heightened negative feedback, and blunted HPA axis responsiveness.
Fundamentally, this means that in those patients observed, cortisol levels are persistently lower than is to be expected. This appears to be traced back to the hypothalamus and pituitary gland becoming somewhat unable to appropriately detect or respond to the low cortisol levels.
Many studies have not just identified this as a fairly consistent finding in ME/CFS but have furthermore observed a correlation between this dysfunction and symptom severity. It is of note however that some studies dispute this finding.
This dysfunction in the HPA axis has been used somewhat deviously by some groups to verify the effectiveness of talking-based therapies such as cognitive behavioral therapy (CBT).
This is in part due to the effectiveness these therapies can appear to have in conditions such as anxiety disorders in which HPA axis dysfunction has also been proven to play a somewhat central role. However such a line of thought, while helpful in many diseases where HPA axis appears to be a disease mediator, is unlikely to be helpful in a disease where the HPA axis does not yet appear to be central.
While there are a large number of studies confirming their independent findings of HPA axis dysfunction, few make the leap to develop a hypothesis for this being the central disease mechanism. This is likely a result of the multitude of other research indicating a deeper physiological defect in ME/CFS of which HPA axis may simply be an unfortunate by-product.
One interesting study that bears thought as to HPA axis dysfunction developing as a secondary condition is a somewhat unrelated study by Dunn et al. This study focuses upon how cytokines can in turn activate the HPA axis, initiating a stress response. Cytokines are a rapidly emerging line of study in ME/CFS and we recently produced an article exploring why they are gaining increased exposure in the ME/CFS research field.
It's an interesting notion that cytokines can directly influence the functioning of the HPA axis. When we consider the emerging results of researchers such as Prof. Lipkin outlining significant cytokine abnormalities in ME/CFS, perhaps we have a logical line of reasoning as to why the HPA axis appears somewhat blunted.
If the observed cytokine abnormalities prove repeatable and appear chronic, then it stands to reason that the HPA axis is under significant strain for a prolonged period of time. This could account for lower cortisol levels as time progresses, alongside a blunting of the HPA axis response when challenged with a stressor.
This hypothesis would also be supported by the HPA axis dysfunction seen in other chronic conditions with significant cytokine disturbance, such as lupus.
Overall, while problems with the adrenal glands and HPA axis function don't yet appear to be a sole causative agent for ME/CFS, they do provide an interesting explanation for certain symptoms of ME/CFS from which patients suffer. As time progresses, and through the thorough research done every day, we learn more and more about the complex interconnections between different organs and systems such as the HPA axis.
The connections between these systems, while seemingly unrelated to many diseases, appear to play quite a substantial role in the symptomolgy of ME/CFS, perhaps tying together with increasing evidence of autonomic dysfunction within ME/CFS.
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.

View the Post on the Blog
Last edited by a moderator:
