Simon
Senior Member
- Messages
- 3,789
- Location
- Monmouth, UK
New, from Michael Maes:
In myalgic encephalomyelitis/chronic fatigue syndrome, increased autoimmune activity against 5-HT is associated with immuno-inflammatory pathways and bacterial translocation
On the face of it, a spectacular finding, with positive autoimmunity in 61% of 117 ME/CFS patients (Fukuda) vs 14% of Chronic Fatigue controls (great comparison group) and 6% of healthy controls. But I would want to read the full text before commenting further. 5-HT is serotonin, an important neurotransmitter.
Abstract
Background
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is accompanied by activation of immuno-inflammatory pathways, increased bacterial translocation and autoimmune responses to serotonin (5-HT). Inflammation is known to damage 5-HT neurons while bacterial translocation may drive autoimmune responses. This study has been carried out to examine the autoimmune responses to 5-HT in ME/CFS in relation to inflammation and bacterial translocation.
Methods
We examined 5-HT antibodies in 117 patients with ME/CFS (diagnosed according to the centers for disease control and prevention criteria, CDC) as compared with 43 patients suffering from chronic fatigue (CF) but not fulfilling the CDC criteria and 35 normal controls. Plasma interleukin-1 (IL-1), tumor necrosis factor (TNF)α, neopterin and the IgA responses to Gram-negative bacteria were measured. Severity of physio-somatic symptoms was measured using the fibromyalgia and chronic fatigue syndrome rating scale (FF scale).
Results
The incidence of positive autoimmune activity against 5-HT was significantly higher (p<0.001) in ME/CFS (61.5%) than in patients with CF (13.9%) and controls (5.7%). ME/CFS patients with 5-HT autoimmune activity displayed higher TNFα, IL-1 and neopterin and increased IgA responses against LPS of commensal bacteria than those without 5-HT autoimmune activity. Anti-5-HT antibody positivity was significantly associated with increased scores on hyperalgesia, fatigue, neurocognitive and autonomic symptoms, sadness and a flu-like malaise.
Discussion
The results show that, in ME/CFS, increased 5-HT autoimmune activity is associated with activation of immuno-inflammatory pathways and increased bacterial translocation, factors which are known to play a role in the onset of autoimmune reactions. 5-HT autoimmune activity could play a role in the pathophysiology of ME/CFS and the onset of physio-somatic symptoms. These results provide mechanistic support for the notion that ME/CFS is a neuro-immune disorder.
In myalgic encephalomyelitis/chronic fatigue syndrome, increased autoimmune activity against 5-HT is associated with immuno-inflammatory pathways and bacterial translocation
On the face of it, a spectacular finding, with positive autoimmunity in 61% of 117 ME/CFS patients (Fukuda) vs 14% of Chronic Fatigue controls (great comparison group) and 6% of healthy controls. But I would want to read the full text before commenting further. 5-HT is serotonin, an important neurotransmitter.
Abstract
Background
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is accompanied by activation of immuno-inflammatory pathways, increased bacterial translocation and autoimmune responses to serotonin (5-HT). Inflammation is known to damage 5-HT neurons while bacterial translocation may drive autoimmune responses. This study has been carried out to examine the autoimmune responses to 5-HT in ME/CFS in relation to inflammation and bacterial translocation.
Methods
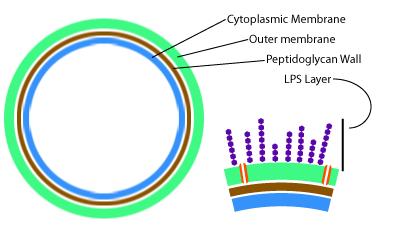
We examined 5-HT antibodies in 117 patients with ME/CFS (diagnosed according to the centers for disease control and prevention criteria, CDC) as compared with 43 patients suffering from chronic fatigue (CF) but not fulfilling the CDC criteria and 35 normal controls. Plasma interleukin-1 (IL-1), tumor necrosis factor (TNF)α, neopterin and the IgA responses to Gram-negative bacteria were measured. Severity of physio-somatic symptoms was measured using the fibromyalgia and chronic fatigue syndrome rating scale (FF scale).
Results
The incidence of positive autoimmune activity against 5-HT was significantly higher (p<0.001) in ME/CFS (61.5%) than in patients with CF (13.9%) and controls (5.7%). ME/CFS patients with 5-HT autoimmune activity displayed higher TNFα, IL-1 and neopterin and increased IgA responses against LPS of commensal bacteria than those without 5-HT autoimmune activity. Anti-5-HT antibody positivity was significantly associated with increased scores on hyperalgesia, fatigue, neurocognitive and autonomic symptoms, sadness and a flu-like malaise.
Discussion
The results show that, in ME/CFS, increased 5-HT autoimmune activity is associated with activation of immuno-inflammatory pathways and increased bacterial translocation, factors which are known to play a role in the onset of autoimmune reactions. 5-HT autoimmune activity could play a role in the pathophysiology of ME/CFS and the onset of physio-somatic symptoms. These results provide mechanistic support for the notion that ME/CFS is a neuro-immune disorder.