Bob
Senior Member
- Messages
- 16,455
- Location
- England (south coast)
Not open access, unfortunately.
A large multi-center study by Klimas, Bateman, Levine, Peterson, Hornig, Komaroff and colleagues.
"This paper introduces the Chronic Fatigue Initiative..."
Findings from a clinical and laboratory database developed for discovery of pathogenic mechanisms in myalgic encephalomyelitis/chronic fatigue syndrome
N.G. Klimas, G. Ironson, A. Carter, E. Balbin, L. Bateman, D. Felsenstein, S. Levine, D. Peterson, K. Chiu, A. Allen, K. Cunningham, C.G. Gottschalk, M. Fletcher, M. Hornig, C. Canning & A.L. Komaroff
Fatigue: Biomedicine, Health & Behavior 2015; 3:75-96
Published online: 24 Apr 2015
DOI:10.1080/21641846.2015.1023652
http://www.tandfonline.com/doi/abs/10.1080/21641846.2015.1023652
A large multi-center study by Klimas, Bateman, Levine, Peterson, Hornig, Komaroff and colleagues.
"This paper introduces the Chronic Fatigue Initiative..."
Findings from a clinical and laboratory database developed for discovery of pathogenic mechanisms in myalgic encephalomyelitis/chronic fatigue syndrome
N.G. Klimas, G. Ironson, A. Carter, E. Balbin, L. Bateman, D. Felsenstein, S. Levine, D. Peterson, K. Chiu, A. Allen, K. Cunningham, C.G. Gottschalk, M. Fletcher, M. Hornig, C. Canning & A.L. Komaroff
Fatigue: Biomedicine, Health & Behavior 2015; 3:75-96
Published online: 24 Apr 2015
DOI:10.1080/21641846.2015.1023652
http://www.tandfonline.com/doi/abs/10.1080/21641846.2015.1023652
Abstract
Background: Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a complex, chronic illness that is often disabling. This paper introduces the Chronic Fatigue Initiative, which conducted a large multi-center study to more fully characterize ME/CFS and ultimately to describe and understand the underlying mechanisms and pathogenesis of this illness.
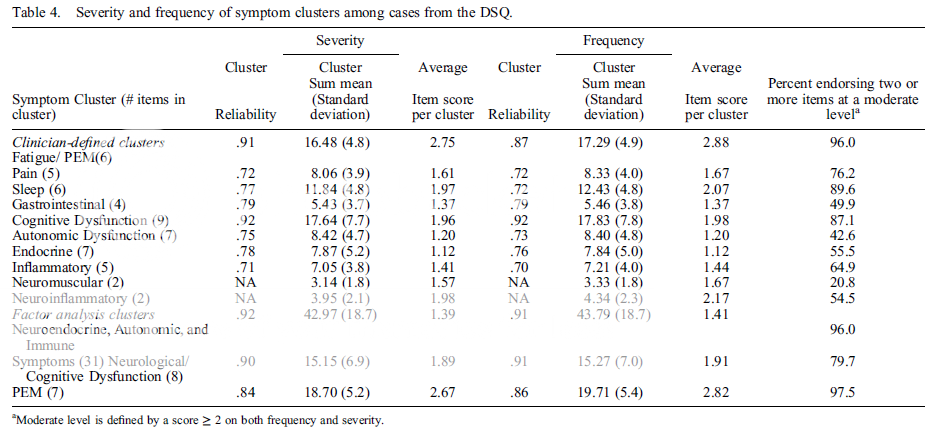
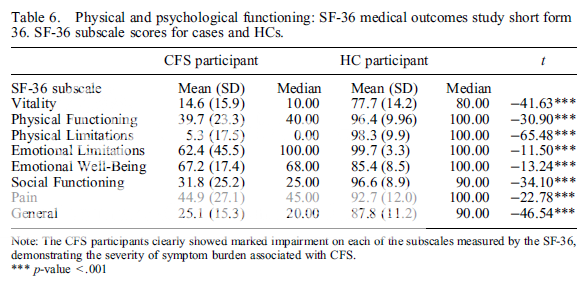
Methods: A total of 203 patients with ME/CFS (cases) and 202 matched healthy controls (HCs) were enrolled from 5 geographically different expert clinical sites to create a well-characterized population linked to a national biorepository. ME/CFS subjects were compared to a one-to-one matched HC population for analyses of symptoms and illness severity. Cases were further evaluated for frequency and severity of symptoms and symptom clusters, and the effects of illness duration and acute vs. gradual onset.
Results: This study collected more than 4000 pieces of data from each subject in the study. Marked impairment was demonstrated for cases vs. controls. Symptoms of fatigue were identified, but also, nearly as frequent and severe, were symptoms of cognitive dysfunction, inflammation, pain and autonomic dysfunction. Potential subgrouping strategies were suggested by these identified symptom clusters: sleep, neurocognitive, autonomic, inflammatory, neuroinflammatory, gastrointestinal and endocrine symptoms.
Conclusions: Clearly, ME/CFS is not simply a state of chronic fatigue. These data indicate that fatigue severity is matched by cognitive, autonomic, pain, inflammatory and neuroinflammatory symptoms as the predominant clinical features. These findings may assist in the clarification and validation of case definitions. In addition, the data can aid clinicians in recognizing and understanding the overall illness presentation. Framing ME/CFS as a multisystem disorder may assist in developing therapies targeting the multifaceted domains of illness.
Last edited: