Even Endo's still can't agree on the upper end of range for TSH test
The sensitivity limitations of the first generation RIA methods precluded detecting the lower euthyroid reference limit (2.5 percentile) whereas upper reference limits (97.5 percentile) were reportedly to be as high as 10 mIU/L. This elevated upper limit primarily resulted from gonadotropin cross-reactivity and the failure to exclude individuals with subclinical autoimmune thyroid disease who have higher TSH values (237,286-288). Using current third generation IMA methodology,
the lower TSH reference limit has now been shown to approximate 0.3 to 0.4 mIU/L (289-291). This estimate appears consistent irrespective of the population studied or the method used (289,290,292-297).
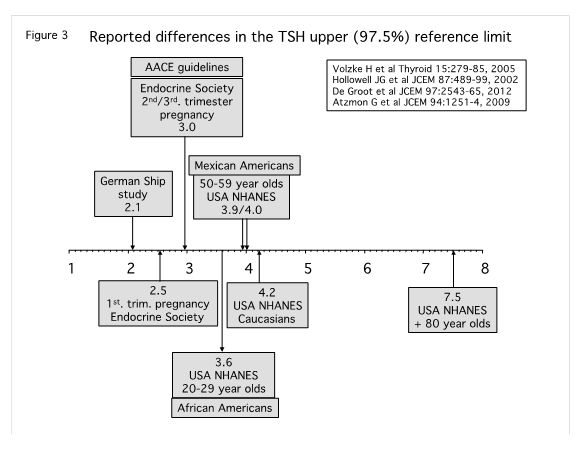
In contrast, the setting of the TSH upper reference limit (97.5 percentile) has become controversial (291,298-301) with estimates ranging from 2.1 mIU/L (295,297) to 7.5 mIU/L (289,299,302)
. Multiple factors influence the calculation of the TSH upper reference limit for a population. These include population demographics like sex (289), ethnicity (289,303-305), iodine intake (306), BMI (307-312), smoking status (303,313,314) and age (302,304,315,316) as well as the failure to exclude the presence of subclinical autoimmune thyroid disease using the presence of TPO antibodies (287,289,317,318).
Recent studies have suggested that TSH increases with age and that a mild TSH elevation in elderly individuals may even convey a survival benefit, although other reports dispute this (299,302,319-324). These reports have led to the suggestion that age-specific TSH reference limits should be considered (315,325). However, it appears that these mild TSH elevations may be transient (326), or in part relate to polymorphisms of the TSH receptor and cannot be interpreted to imply that subclinical hypothyroidism per se is necessarily advantageous for elderly individuals (321,327,328). Whereas there appears to be a positive correlation between age and TSH concentrations in iodine sufficient populations (289,299,329) the opposite is the case for iodine deficient populations in which there appears to be no TSH increase with age, or even a decline (286,295,296,330,331). In areas of iodine sufficiency the correlation between increasing TSH and age could represent a failure to exclude subjects with autoimmunity who may, or may not, be detected by a positive TPOAb test (317,332,333). Complicating these questions is the fact that current TSH IMAs differ in specificity for recognizing circulating TSH isoforms and that this can give rise to a full 1.0 mIU/L difference in TSH values reported by different assays – a difference that in some cases is greater than the influence of many of the other variables listed above (31,296,334,335). Because hypothalamic TRH modulates TSH molecular glycosylation and biologic activity, a rise in TSH with age could represent an increase in the secretion of biologically inactive TSH, yet immunologically detected isoforms (336,337). The blunting of the TSH response to TRH and decreased amplitude of the TSH nocturnal peak would be consistent with this premise (338,339). In contrast, in areas of iodine deficiency the inverse relationship between TSH and age could represent a failure to exclude individuals with autonomously functioning nodules (332).
The TSH upper reference limits for non-pregnant subjects remains a contentious issue, such that it is difficult for manufacturers to cite a TSH reference range appropriate for universal adoption across different populations in different geographic areas (Figure 3).
This has led to guidelines proposing the adoption of an empiric TSH upper limit of 2.5 -3.0 mIU/L, which is in accord with the TSH interval associated with the lowest prevalence of thyroid antibodies (13,37,228,317). Furthermore, a TSH upper limit between 2.0 and 3.0 mIU/L would also be appropriate for reproductive age women and pregnancy, in whom current guidelines now recommend using 2.5 mIU/L for preconception planning and the first trimester, and 3.0 mIU/L as the upper limit for the second and third trimesters (13,39,40,203,228,288,340).
The adult TSH population reference range does not apply to neonates or children. Serum TSH values are generally higher in neonates and then gradually decline until the adult range is reached after puberty (198,296,341-346). This necessitates using age-specific TSH reference ranges for diagnosing thyroid dysfunction in these pediatric age categories.