View the Post on the Blog
View the Post on the Blog
The first in a new series of (mercifully) short pieces on recent research. By Simon McGrath
A new study used data from the large PACE Trial to see if CBT and Graded exercise (GET) improved ME/CFS pain. (The main trial itself found a moderate effect of CBT and GET on self-reported fatigue and function.) The study looked at muscle and joint pain frequency, and fibromyalgia status. And it compared CBT and GET to both specialised medical care (SMC) and APT (pseudo-pacing).
The questions are, did CBT or GET have any effect on these - and if so, how big was the effect? The answers were unimpressive:
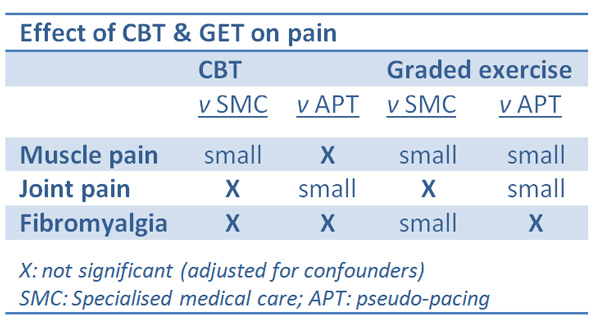
So CBT helped a little with muscle pain compared with SMC (but not APT), a little with joint pain compared with SMC (but not APT), and not at all with fibromyalgia. Graded exercise fared a little better, but the effect was small at best.
What does a 'small' effect mean?
How small is small? For muscle and joint pain, the study used 'Cohen's d' to measure the effect of the treatments, and the values ranged from 0.24 to 0.31. Generally, 0.2 is considered a small effect, 0.5 is moderate and 0.8 is large (over 1 is very large), but the best way to gauge size is to look at a graph of the data for control vs treatment. The graph below shows an effect size of 0.27, typical in this study. The control group is in red, the treatment group - showing a small improvement effect (lower score) - is in black. The shaded pink area shows the overlap between the two groups. As you can see, there is a definite treatment effect overall, but it's rather a small one.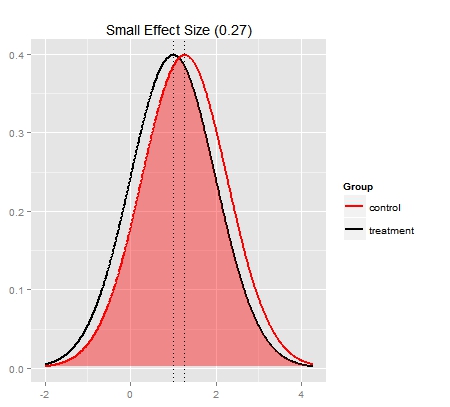
The effect on Fibromyalgia status needs to be measured slightly differently, so the authors used the "Number Needed to Treat" measure. On average, 12 patients need to be treated with GET for one patient to no longer meet the criteria for fibromyalgia. This too is a small effect (note it may be a case of moving from 'just meeting' the criteria, to 'just not meeting criteria', rather than recovery).
No evidence on effect on pain severity
Disappointingly, the study only measured pain frequency, not pain severity, with the authors acknowledging this approach "may not be as clinically meaningful" as using both pain frequency and severity. Many patients with severe pain would agree. Note that as this was an outpatient study, the severely affected - who often have the worst pain - were excluded.
Treatment effects on pain were independent of ‘change in fatigue’.
You might expect that if CBT and graded exercise helped patients recover then symptoms would improve across the board. But surprisingly, the study found that gains in pain were not linked to improvements in fatigue.
Summary
CBT and Graded Exercise had a small or insignificant effect on muscle and joint pain frequency, and Fibromyalgia in the PACE Trial. There was no evidence on the ability of CBT and Graded exercise to reduce pain severity.
Read more on the Phoenix Rising thread about this study
This article first appeared on the ME Association's website
Simon McGrath tweets on ME/CFS research
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. and we'd love to expand our Board of Directors. So, if you think you can help then please contact Mark through the Forum.
And don't forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
View the Post on the Blog

