Tom Kindlon
Senior Member
- Messages
- 1,734
Stress management skills, neuroimmune processes and fatigue levels in persons with chronic fatigue syndrome.
Lattie EG, Antoni MH, Fletcher MA, Penedo F, Czaja S, Lopez C, Perdomo D, Sala A, Nair S, Fu SH, Klimas N.
Brain Behav Immun. 2012 Aug;26(6):849-58. doi: 10.1016/j.bbi.2012.02.008. Epub 2012 Mar 6.
Abstract*
OBJECTIVES:
Stressors and emotional distress responses impact chronic fatigue syndrome (CFS) symptoms, including fatigue.
Having better stress management skills might mitigate fatigue by decreasing emotional distress.
Because CFS patients comprise a heterogeneous population, we hypothesized that the role of stress management skills in decreasing fatigue may be most pronounced in the subgroup manifesting the greatest neuroimmune dysfunction.
METHODS:
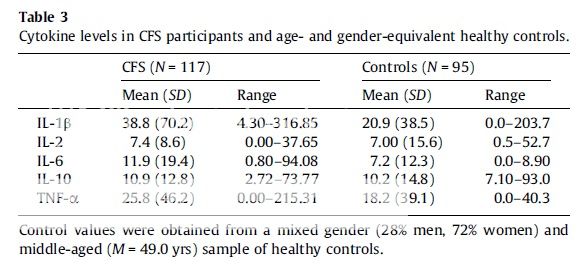
In total, 117 individuals with CFS provided blood and saliva samples, and self-report measures of emotional distress, perceived stress management skills (PSMS), and fatigue.
Plasma interleukin-1-beta (IL-1β, IL-2, IL-6, IL-10, and tumor necrosis factor-alpha (TNF-α), and diurnal salivary cortisol were analyzed.
We examined relations among PSMS, emotional distress, and fatigue in CFS patients who did and did not evidence neuroimmune abnormalities.
RESULTS:
Having greater PSMS related to less fatigue (p=.019) and emotional distress (p<.001), greater diurnal cortisol slope (p=.023) and lower IL-2 levels (p=.043).
PSMS and emotional distress related to fatigue levels most strongly in CFS patients in the top tercile of IL-6, and emotional distress mediated the relationship between PSMS and fatigue most strongly in patients with the greatest circulating levels of IL-6 and a greater inflammatory (IL-6):anti-inflammatory (IL-10) cytokine ratio.
DISCUSSION:
CFS patients having greater PSMS show less emotional distress and fatigue, and the influence of stress management skills on distress and fatigue appear greatest among patients who have elevated IL-6 levels.
These findings support the need for research examining the impact of stress management interventions in subgroups of CFS patients showing neuroimmune dysfunction.
*Each sentence has its own paragraph