New material about DSM-V (DSM-5) Somatic Symptom Disorder Work Group presentations
New material about DSM-V (DSM-5) Somatic Symptom Disorder Work Group presentation slides
(A version of this posting was published on Co-Cure on 19 January and also appears on
DSM-5 Watch.)
The American Psychiatric Association (APA), publishers of the DSM, now plans to publish draft proposals for changes to its diagnostic categories on
10 February. [1]
Comments will be accepted for a "two to three month" public consultation and reviewed by the relevant DSM-V Work Groups. There is no information up on the site yet about the consultation process for this first draft.
According to Dr Todd Finnerty, sources close to the Task Force have said that the APA may launch its new DSM-V website prior to 10 February, in order to test the webages.
Those of us with an interest in corporate identity and house style, may have noticed that the APA's 10 December Press Release had used "DSM-5" not "DSM-V" and in a piece titled
Why is DSM-5 Being Delayed (1 January) APA President, Alan F Schatzberg, had also used "DSM-5" throughout. Which might suggest that the APA may be intending to drop the use of Roman numerals for the forthcoming edition.
Other than via journal editorials, no updates have been issued by any of the DSM-V Work Groups since April, last year.
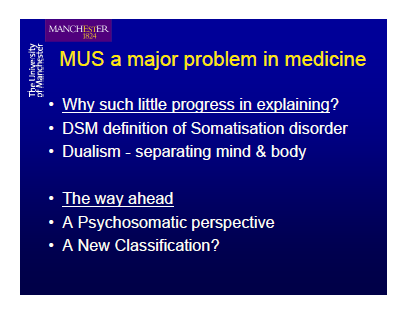
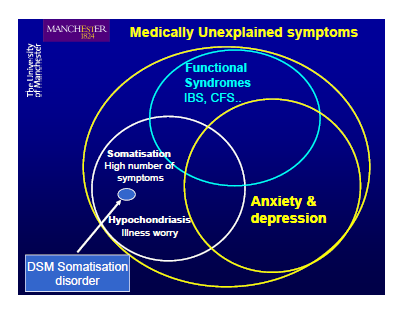
The DSM-V Work Group for "Somatic Symptom Disorders" that is revising categories currently classified under DSM-IV "Somatoform Disorders" has been exploring the potential for eliminating criteria such as
"medically unexplained symptoms" in order to
"diminish the dichotomy" between disorders based on
"medically unexplained symptoms and patients with organic disease."
The conceptual framework the Somatic Symptom Disorders Work Group were proposing, in June 09, would
"...allow a diagnosis of somatic symptom disorder in addition to a general medical condition, whether the latter is a well-recognized organic disease or a functional somatic syndrome such as irritable bowel syndrome or chronic fatigue syndrome." [2]
DSM-V SSD Work Group presentation slides
In November '09,
The Academy of Psychosomatic Medicine, the Organization for Consultation and Liaison Psychiatry and publishers of Psychosomatics, held its 56th Annual Meeting in Nevada. [3]
This Annual Meeting received "significant financial support" from sponsor drug companies:
AstraZeneca Pharmaceuticals, Bristol-Myers Squibb and Otsuka Pharmaceutical, Inc., Eli Lilly and Company and
Ortho-McNeil Janssen Scientific Affairs, LLC.
Three members of the DSM-V Somatic Symptom Disorders Work Group,
Francis Creed,
Lawson Wulsin and
Chair, Joel Dimsdale, gave presentations around "Medically Unexplained Symptoms" (MUS) and DSM-V, and around DSM-V proposals and progress.
Links for PDFs for the Creed and Wulsin presentations slides are appended. Text only for the Dimsdale presentation is available, and I have also appended this.
This material, from November, represents the most recent information around the deliberations of the DSM-V Work Group that is revising the categories currently coded under DSM-IV "Somatoform Disorders".
When the APA publishes its proposals for changes to its diagnostic categories these will be posted as soon as they are available on my new
Dx Revision Watch site at:
http://dxrevisionwatch.wordpress.com
For a Table setting out Current DSM-IV Codes and Categories for Somatoform Disorders and their ICD-10 Equivalents, and for more in depth information on the deliberations of the Somatic Symptom Disorders Work Group, so far, see:
DSM-5 Watch page: DSM-5 proposals 2:
http://wp.me/PKrrB-hT
From the American Psychiatric Association's (APA) 10 December press release:
APA will continue to work with the WHO to harmonize the DSM-5 with the mental and behavioral disorders section of the ICD-11. Given the timing of the release of both DSM-5 and ICD-11 in relation to the ICD-10-CM, the APA will also work with the CDC and CMS to propose a structure for the U.S. ICD-10 CM that is reflective of the DSM-5 and ICD-11 harmonization efforts."
Note: I have contacted The Academy of Psychosomatic Medicine to ask whether transcripts or notes for the first two presentations are available or are going to be made available in the future, in order that the slides might be better put into context. I have been told that transcripts are not available and that I would need to contact Francis Creed and Lawson Wulsin, directly.
Presentations:
The Academy of Psychosomatic Medicine
Bethesda, Maryland, US
The Organization for Consultation and Liaison Psychiatry
Publishers of Psychosomatics
2009 ANNUAL MEETING in LAS VEGAS
November 11-14, 2009
56th Annual Meeting
Award Lectures
Hackett Award - Friday, 12:45pm - 1:45pm
Francis Creed, MD, FRCP:
Can We Now Explain Medically Unexplained Symptoms? [4]
PDF Creed Presentation Slides (No transcript)
http://www.apm.org/ann-mtg/2009/presenter-slides/HackettAward-creed.pdf
PDF References
http://www.apm.org/ann-mtg/2009/presenter-slides/HackettAward-creed-refs.pdf
(This is a lengthy but important presentation by DSM-V SSD Work Group member, Francis Creed. It is unfortunate that a transcript is not available but please view the slides - there are many references to "Chronic fatigue syndrome", chronic fatigue and IBS and to the so-called "Functional Somatic Syndromes".)
Workshops
Workshop 15 - Saturday, 1:45 - 2:45pm
DSM-V for Psychosomatic Medicine: Current Progress and Controversies
Lawson Wulsin, MD, FAPM,
DSM V for Psychosomatic Medicine: Current Progress and Controversies [5]
PDF Wulsin Presentation Slides (No transcript)
http://www.apm.org/ann-mtg/2009/presenter-slides/W15-wulsin.pdf
Joel Dimsdale, MD, FAPM,
Update on DSM V Somatic Symptoms Workgroup [6]
Text version (No slides)
http://www.apm.org/ann-mtg/2009/presenter-slides/W15-dimsdale-text.pdf
[Text version]
Update on DSM V Somatic Symptoms Workgroup
Workshop #15, APM Annual Meeting, 11-14-09
DSM-V for Psychosomatic Medicine: Current Progress and Controversies
The Somatic Symptoms Workgroup was charged with reviewing most somatoform disorders, psychological factors affecting medical condition, and factitious disorders. There is considerable confusion regarding the diagnostic terminology and a reluctance to use these diagnostic labels. In addition to relying on expert opinion and the research literature, the Workgroup has also been conducting studies in an effort to learn how physicians actually use these diagnostic labels.
These diagnoses are rarely coded. In a study of >1,000,000 Virginia Anthem Blue Cross policy holders, Levenson found that there were fewer than 600 patients with such disorders. [7] Of these 600 patients, the largest group of patients were diagnosed with Psychological Factors Affecting Medical Condition.
Four focus groups were held in San Diego and Edinburgh. Psychiatrists from very different practice settings attended these groups (child psychiatrists, forensic psychiatrists, psychopharmacologists, consultation psychiatrists, psychotherapists). Nonpsychiatrist attendees included neurologists, pediatricians, and gastroenterologists. Using themes identified from the focus groups, an anonymous internet poll was designed. Using mailing lists from a variety of professional organizations, physicians were invited to respond to an anonymous poll.
Three hundred thirty-two physicians responded to the poll. Two thirds were psychiatrists; two-thirds were from the United States. While in general, physicians reported that somatoform patients were relatively rare in their practices (i.e. 0-2%), some physicians reported high prevalence of these patients. Over 30% of the physicians regarded the diagnostic guidelines for pain disorder and somatoform disorder not otherwise specified as "unclear." Similar numbers of doctors regarded these particular disorders as "not useful." Physicians were uniform in their opinion that patients disapproved of such diagnostic labels. Respondents also felt that there was a great deal of overlap between somatization disorder, pain disorder, hypochondriasis, and somatoform disorder not otherwise specified. In addition, they felt that that there was overlap between the somatoform disorders and anxiety and depressive disorders.
The Somatic Symptoms Workgroup has been struck by the fact that "medically unexplained symptoms" (MUS) comprise the crucial intellectual underpinning of the large group of somatoform disorders; yet MUS designations are perilous. They foster mind-body dualism; they confuse "undiagnosed" with "unexplained"; they contribute to doctor-patient antagonism; and they base a diagnosis on a negative, rather than positive criteria.
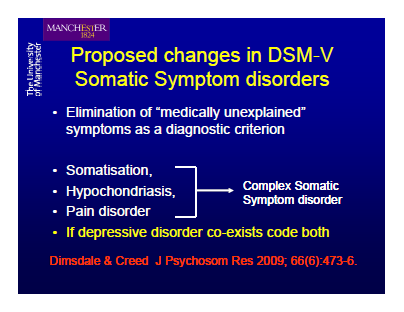
The Workgroup is proposing a series of changes to these disorders. First off, such disorders would be grouped together under one rubric entitled "Somatic Symptom Disorders", which would include somatoform disorders, factitious disorders, and psychological factors affecting medical condition. Second, because of their many common features, the group is proposing that hypochondriasis, pain disorder, somatization disorder, and undifferentiated somatoform disorder be grouped together as "Complex Somatic Symptom Disorder", with optional specifyers to designate when the predominant presentation is, for instance, hypochondriasis, etc. MUS is de-emphasized for this diagnosis, which would require both prominent somatic symptoms causing distress or dysfunction, as well as positive psychological criteria (behavior, cognition, perception).
A draft description of these and other disorders will be published on the APA's DSM V website in January, 2010.*
In addition, a paper describing the thinking of the workgroup and providing a slightly earlier version of the diagnostic guidelines may be found at:
Dimsdale J , Creed F, and on behalf of the DSM-V Workgroup on Somatic Symptom Disorders. The proposed diagnosis of somatic symptom disorders in DSM-V to replace somatoform disorders in DSM-IV-a preliminary report, J Psychosom Res, 66 (2009) 473-476
The workgroup welcomes comments from colleagues about the proposed changes. Are the proposed changes on the right track? Does this proposal represent, all in all, a step forward? Are there major adverse unintended consequences? Workgroup members include: Arthur Barsky, Francis Creed, Javier Escobar, Nancy Frasure-Smith, Michael Irwin, Frank Keefe, Sing Lee, James Levenson, Michael Sharpe [8], Lawson Wulsin, Joel Dimsdale (chair).
Please send comments to Joel Dimsdale via email
jdimsdale@ucsd.edu .
[Text version Dimsdale Presentation Ends]
[1] American Psychiatric Association, DSM-V: The Future Manual
http://www.psych.org/MainMenu/Research/DSMIV/DSMV.aspx
[2] Editorial: Dimsdale J , Creed F, and on behalf of the DSM-V Workgroup on Somatic Symptom Disorders. The proposed diagnosis of somatic symptom disorders in DSM-V to replace somatoform disorders in DSM-IV - a preliminary report, J Psychosom Res, 66 (2009) 473-476
http://www.jpsychores.com/article/S0022-3999(09)00088-9/fulltext
[3] The Academy of Psychosomatic Medicine 2009 ANNUAL MEETING November 11-14, 2009, Las Vegas.
http://www.apm.org/ann-mtg/2009/index.shtml
[4] Francis Creed, MD, is a member of the DSM-V Somatic Symptom Disorders Work Group (aka Somatic Distress Disorders Work Group) and was a member of the international CISSD Project, co-ordinated by Dr Richard Sykes, PhD. Francis Creed is a co-editor of the Journal of Psychosomatic Research.
[5] Lawson R. Wulsin, MD, is a member of the DSM-V Somatic Symptom Disorders Work Group.
[6] Joel E Dimsdale, MD, chairs the DSM-V Somatic Symptom Disorders Work Group, is a member of the DSM-V Task Force and was a member of the CISSD Project.
[7] James L Levinson, MD, is a member of the DSM-V Somatic Symptom Disorders Work Group and was a member of the CISSD Project.
[8] Michael Sharpe, MD, Director, University of Edinburgh Psychological Medicine Research Group, is a member of the Somatic Symptom Disorders Work Group, a co-PI of the UK MRC funded PACE Trial and was a member of the CISSD Project.
Related information:
The current use of the diagnosis "Psychological Factors Affecting Medical Condition" in DSM-IV is set out here:
http://www.behavenet.com/capsules/disorders/psyfactorsmedcon.htm
Francis Creed is currently working with EACLPP colleagues, Henningsen and Fink, on a draft white paper for the EACLPP MUS Study Group called:
"Patients with medically unexplained symptoms and somatisation - a challenge for European health care systems". A copy of the MUS Study Group working draft can be downloaded from the EACLPP site:
http://www.eaclpp.org/documents/Patientswithmedicallyunexplainedsymptomsandsomatisation.doc
The January 2010, Editorial
"Is there a better term than "Medically unexplained symptoms?" Creed F, Guthrie E, Fink P, Henningsen P, Rief W, Sharpe M, White P. J Psychoso Res: Volume 68, Issue 1, Pages 5-8, discusses the deliberations of the EACLPP study group. The Editorial also includes references to the DSM and ICD revision processes. (Subscription or payment required)
Javier Escobar, MD, Director of the University of Medicine and Dentistry of New Jersey (UMDNJ) - Robert Wood Johnson Medical School (RWJMS) Medically Unexplained Physical Symptoms (MUPS) Research Center, which has been supported with over $4M in funding by the US National Institute of Mental Health (NIMH), is a member of the DSM-V Task Force. Dr Escobar serves as a Task Force liaison to the Somatic Symptom Disorders Work Group and works closely with this group.
2008 Special Report by Marin and Escobar:
"Unexplained Physical Symptoms What's a Psychiatrist to Do?" Psychiatric Times. Vol. 25 No. 9, August 1, 2008:
http://www.psychiatrictimes.com/display/article/10168/1171223