View the Post on the Blog
View the Post on the BlogJoel (Snowathlete) continues his series on zoonotic pathogens with a thorough examination of Borellia and Lyme disease - and their possible relevance for ME/CFS patients.
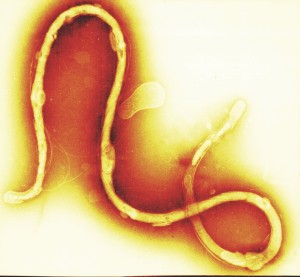
Borrelia spirochete
by Tina Carvalho, University of Hawaii at Manoa
Borrelia is the bacterium that causes borreliosis. It is a microscopic spiral-shaped parasite. There are many different species of Borrelia, some of which cause Lyme borreliosis, otherwise known as Lyme disease.
Borrelia is a zoonotic pathogen transmitted via a vector, usually a tick. There is evidence that other arthropods such as fleas, biting flies, mites and spiders also carry it, but so far there is only limited - mainly anecdotal - evidence of transmission to humans by non-tick arthropods.
Transmission from ticks appears to be the most common and important method of transmission, perhaps because ticks have a salivary protein called Salp15 which the Borrelia attaches to and which is thought to have immunosuppressive effects [1]. Following transmission, Borrelia can travel through the body quite rapidly, including into the central nervous system [2, 3].
How common is it?
Borreliosis, including Lyme and Lyme-like diseases, is one of the most prevalent infectious diseases in the world. In the USA it is the most commonly-reported vector-borne disease and the sixth most common disease nationally. It is more prevalent in the northeast and upper Midwest of the US; in Massachusetts, only hepatitis and HIV-AIDS are more common, despite under-reporting.

Deer Ticks (Ixodes scapularis)
Photo by Sandy__R
In the past there has been a view that tick-borne infections, particularly Borrelia, are only common in the US and that other parts of the world don’t have a problem. This is simply not the case, with the UK, mainland Europe and Asia/Oceania also affected. The disease is the same, the ticks (and often the species of Borrelia) are different.
The existence of Lyme disease in Australia is controversial. The government has strict border controls to stop foreign insects and pathogens from entering the country, and the government have been reluctant to accept that there is a local problem, claiming that Borrelia infection occurs outside the country when people travel abroad. Most Lyme organizations in Australia dispute this and so does some of the medical literature [4].
Different strains
In North America, the predominant strain that causes Lyme disease is Borrelia burgdorferi. This strain also occurs in Europe and Asia, though B. garinii and B. afzelii are more common in these areas. Many other strains are known to infect humans and cause disease, some being suspected of causing Lyme, or Lyme-like illness. In particular, two other strains; B. spielmanii and B. bavariensis (both closely related to B. burgdorferi) are now widely acknowledged to cause Lyme disease.
Some strains have only been confirmed to cause borreliosis in the last few years, but have possibly been doing so for much longer[5].
Co-infections
Those diagnosed with Lyme disease often have co-infections, usually transmitted by the same tick that gave them Borrelia, and these co-infections can complicate disease and treatment. Some of the more common co-infections are Babesia, Rickettsia, Ehrlichia and Bartonella, and they can be serious in their own right. It is common for ticks to transmit multiple pathogens in one bite. Some of these other pathogens will be discussed in detail in future articles in the zoonotics series.
Symptoms
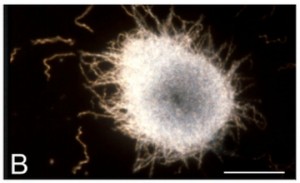
Borrelia spirochete agglomeration into colony-like masses.
Image courtesy of BioMed Central.
When you peruse a list of symptoms caused by Lyme disease or other borreliosis, you can’t help but notice that most of the symptoms in the list are the same, or similar, to those belonging to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and fibromyalgia.
As with ME/CFS the disease tends to get worse over time with new symptoms developing. A quick Google search will return many pages with information on symptoms. As most readers will be familiar with the majority of these symptoms already, I won’t try to list them here. Instead, I will focus on those symptoms that are usually distinguishable from ME/CFS, though not everyone with Lyme disease will have these symptoms.
Having any of the above may signal that you have Lyme rather than ME/CFS, though not having them doesn't necessarily rule out Lyme.
- Lyme can cause paralysis of facial muscles, sometimes called Bell’s palsy. It tends to be on only one side of the face and often is not permanent.
- Meningitis may also develop from Lyme, or from other forms of borreliosis, and is another symptom which is not as common in ME/CFS.
- Atrophy of the skin may occur, especially with treatment as the Borrelia rise to the peripheral circulation to avoid antibiotic contact.
The other species of Borrelia that cause non-Lyme borreliosis tend to produce milder symptoms, the main presentation being relapsing fever or short-term virus-like illness, but some strains such as B. miyamotoi can, in some cases, cause severe disease [5].
Borrelia's effect on the immune system and its ability to change form
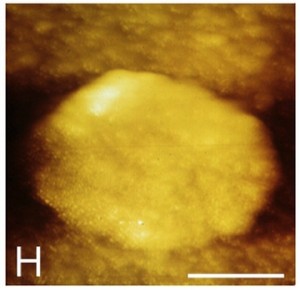
Borrelia cysti, covered by a thick membrane masking the contents of the cyst.
Image courtesy of BioMed Central.
Borrelia is reported to spread quickly to the central nervous system [2, 3] where it is harder to touch, and it is thought that the longer you’ve had it, the harder it is to get antibiotics to these places to kill it.
Genetically speaking, Borrelia is a very advanced bacterium [6]. It is pleomorphic, which means that it can change form from a spirochete to a cell-wall-deficient L-form [25] which is thought to be a mechanism of defense and antibiotic resistance [7, 8]. There is also evidence that Borrelia is able to create biofilm[9] which is thought to provide resistance to antibiotics and immune cells.
Borrelia is the only bacterium with 21 plasmids (B. burgdorferi), which gives it a diverse arsenal. Plasmids are pieces of DNA separate from the chromosomal nucleus of the cell, and they express surface-proteins that are essential to the bacteria’s pathogenicity [10].
Ötzi the Iceman
The remains of Ötzi the Iceman, a deceased human discovered in the Alps in 1991, were found to be infected with Borrelia burgdorferi [11, 12], showing that the bacteria has been infecting humans for at least 5300 years.
Nevertheless, there is some suggestion that Lyme disease has become more pathogenic recently as cases have increased so much in the last 50 years. This may in fact be down to improved recognition and reporting, but there is another theory that it is related to changes in the environment that have favored ticks.
Another interesting view is that Lyme may cause autoimmunity [13,14,15], which is interesting because autoimmune diseases appear to have been on the increase in the modern age as well, and some people believe ME/CFS to be an autoimmune disease (see my previous article here). Perhaps it is possible that Borrelia may be a trigger for ME/CFS autoimmunity?
How is it tested?

Otzi the Iceman - not your typical Lyme disease sufferer
You’d think that as they managed to detect Borrelia in Ötzi, a guy who’s been dead for more than five millennia, it should be a simple matter to detect it in living patients in the here and now, but it isn’t, and as a result the testing of Lyme disease is controversial.There are many who believe that Lyme tests often produce false-negatives, though some disagree about this, and then there is the question of false-positives too... So who is right?
A recent argument for the reliability of tests (at least with established infections) is made by John J Halperin et al [16].However,there are those in the Lyme community that disagree with the science behind many of the conclusions in this article, and they may be right on some points. A key fact, I think, is that the Centers for Disease Control and Prevention (CDC) still says that Lyme diagnosis should not be based solely on test results, which does support the view that the tests are not reliable enough.
Questions aside over the reliability of the approved tests, there is evidence that those who are immunocompromised are more likely to turn up false-negatives for Lyme as the FDA approved tests look for antibodies. The problem is that those with a compromised immune system may not produce antibodies properly [17]. This could therefore be relevant for those of us with ME/CFS because of the evidence of immune dysfunction.
The FDA approved tests
The FDA currently recommends a two-step test process using two different types of test. If the patient is positive or equivocal in the first test then the second test is carried out. If either test is negative then the tests indicate that the patient does not have Lyme disease.
The first test is an enzyme-linked immunoassay (ELISA), which looks for antibodies against Borrelia in the blood. The second test is known as a western blot and looks for immunoglobulin M (IgM) and/or immunoglobulin G (IgG) antibodies.
The results of the approved western blot tests are themselves contentious, as the results that are returned have to be interpreted and the CDC seems to be quite conservative about what constitutes a positive result. Therefore, some people believe that some results that the CDC would deem negative should in fact be read as positive.
Non-approved tests
There are several non-approved tests, some using blood, some using other fluids, some looking for DNA, others for antibodies or antigens. But what is consistent is that they all cost money and because they are not FDA approved you may question their reliability, and even if you don’t, your doctor probably will. Some of the alternative tests on the market have at least been formally assessed and so you may find such published papers [18] useful in making your own judgment on the value of such tests.
Rather than trying to make such a judgment for you or trying to produce an exhaustive list, instead I am just going to mention some of the more commonly recommended tests, though I personally have no experience with any of these tests myself.
Infectolabs in Germany are often suggested, and seem to find a number of people positive who had previously tested negative using the FDA approved tests. Another lab often recommended is IgeneX in the US which also offers a variety of different tests for Borrelia.
Chronic Lyme
Chronic Lyme (or ‘post treatment Lyme disease syndrome’ as the CDC prefers to call it) is controversial. At the heart of it are two opposing organizations and the only thing they have in common is the letters they share in their acronyms. Although it may sound like the title of a bad B movie, a paper titled “Lyme disease: the next decade” [19] does a good job of explaining the differences between these two groups, but I will briefly summarize it here:
Representing the dark-side in our little B movie, we have the Infectious Diseases Society of America (IDSA) who essentially state that chronic Lyme doesn’t exist and have tried to limit treatment of the condition. Representing the light-side you have the International Lyme and Associated Diseases Society (ILADS – remember: the one with the L in the acronym is on the light-side) who speak up for the many thousands of people who have difficulty recovering from Lyme, even after treatment.
This study [20], which supports the views of the IDSA, claims that chronic Lyme doesn’t exist. Nevertheless, the evidence to the contrary is not insignificant, and there has even been litigation against the IDSA alleging conflicts of interest that may have influenced their position on chronic Lyme.
The thing is, it’s all too easy to dismiss an illness like this, isn’t it? That is, unless you're the guy suffering from it, in which case you know all too well how real it is.
Whatever the reason - unidentified infection, bacterial remnants, autoimmunity, irreversible damage - I believe these people are sick, and just like ME/CFS, the illness is not given the attention it deserves.
How is Lyme disease treated?

lone-star tick (Amblyomma americanum)
by Elizabeth Nicodemus
Unsurprisingly, treatment is controversial too, with some believing that longer and stronger treatment is needed, especially in long established illness.
One of the important factors here is that Borrelia is known to replicate slowly, often only once or twice in 24 hours, whereas a bacterium such as staphylococcus (mentioned in my first article on zoonotics) would replicate around 70 times in 24 hours. This is important because many antibiotics target the cell wall of bacteria when they are dividing.
Antibiotics are bactericidal (they kill bacteria) or bacteriostatic (they inhibit replication), so bacteriostatic antibiotics given in short courses may not reduce Borrelia infection very much. Bactericidal antibiotics are probably better against Borrelia, but still the argument is made that low dose and short-course treatments are insufficient to kill most of the infection. This leads to some experts stating that long-term antibiotic treatment is required to control or eradicate Borrelia.
Those that are immunosuppressed by another illness can have more difficulty eradicating Borrelia and so it seems reasonable to suspect that anyone with both Borrelia and ME/CFS would have difficulty with treatment. Additionally, someone with Lyme may be more susceptible to ME/CFS and probably other illnesses, due to the immune impact of Lyme.
Different antibiotic treatments may be given to target Borrelia in its various guises and stages of illness. The treatment of choice is usually doxycycline, but other antibiotics including penicillin, amoxicillin and cefuroxime axetil are also commonly prescribed. In more stubborn cases cefotaxime or ceftriaxone may be given intravenously. Treatment in pregnancy is usually with erythromycin.
As well as ceftriaxone, minocycline or metronidazole may be used where infection of the brain is suspected as it crosses the blood-brain barrier. Additionally, there is evidence that metronidazole may be more effective against Borrelia in its cyst form [21].
What has this to do with ME/CFS?
Some people think that ME/CFS is actually undiagnosed Lyme. There is some limited evidence for that, such as a study from Poland which found that 50 percent of patients diagnosed with borreliosis or tickborne encephalitis could be identified as having CFS, concluding: "The findings suggest that the chronic fatigue syndrome is frequent among patients with a history of borreliosis."[22]. This illustrates that tickborne zoonotics may be implicated in ME/CFS. Alternatively, it could be argued that this is just a result of the two illnesses presenting with similar symptomology.
Another study looked at gender differences and found that women were significantly more likely to develop chronic Lyme compared to men [23]. This is interesting, given the higher ratio of women to men with ME/CFS. Of course, correlation does not constitute evidence, and the finding may support other conclusions, such as the higher degree of women with autoimmune diseases.
A recent study provides evidence which suggests the two diseases are distinct by demonstrating that the cerebrospinal fluid was different in the two conditions [24].
As you can imagine, both sides continue to argue over whether the two illnesses are the same, related, or completely separate. I’m not sure there is enough evidence either way yet, but what is certain is that some people with ME/CFS do later turn out to have Lyme disease. In the last two months on the Phoenix Rising forum I have noticed at least three recent posts (Jan-Feb 2013) from ME/CFS sufferers who have been tested for Lyme and come up positive.
Then you have to bear in mind that Lyme is caused by several different species of Borrelia, as explained above, and several other species are suspected of causing Lyme. Each comes with its own flavor of Lyme disease, where symptoms differ slightly. Additionally, as stated earlier, some people infected with Borrelia don’t get Lyme disease but get other borreliosis illnesses, some of which come with overlapping symptoms to ME/CFS, or which may be present as co-infections.
And importantly, if the illnesses are distinct, then there is still no rule that says you can’t have ME/CFS and Lyme disease at the same time.
Not all species of Borrelia are tested for, and probably not all are even discovered yet, as most have only been discovered in the last two decades. Indeed, the Australian government agree that another pathogen infecting Australian ticks, either a novel Borrelia or some other zoonotic, may be the cause of Lyme-like disease in the country, so there is still room for a greater number of people to have Lyme, borreliosis, or some other tick-borne pathogen as the cause of their ME/CFS, or at least as a co-infection.
Whereas there is some scope for ME/CFS to turn out to be caused by Borrelia, I don’t think anyone can reasonably make that kind of claim yet. For the moment it is categorized as a different illness. Nevertheless, I think the similarities are quite intriguing and at the very least some people labeled as having ME/CFS do have Lyme either instead of, or as well as, ME/CFS. I think it is good, therefore, that some ME/CFS doctors do test for it, and adjust their treatment protocols accordingly. Lerner, De Meirleir, probably one or two others, but it does appear that some ME/CFS doctors overlook it.
What should I do then? Get tested?
With the symptoms being similar and with the knowledge that some people with a diagnosis of ME/CFS do later test positive for Lyme, it has to be said that there is a case for getting tested. Most of us would probably bite your Borrelia-infested arm off if we could swap from an illness of unknown etiology to one of proven etiology, with some prospect of treatment.
The level of testing you go to is of course a different topic and there are no easy answers on how far you should pursue it, but it would seem prudent to at least have the standard FDA approved tests, and if you live in a region where Lyme is endemic, or you think you have some other reason to suspect that you might have been bitten, then you may want to explore test options further.
Joel was diagnosed with ME/CFS in 2009 but struggled with the illness for some time prior to this. He loves to write, and hopes to regain enough health to return to the career he loved and have his work published.
OTHER ARTICLES BY THIS WRITER:
REFERENCES:
- Zoonotics - a load of cock and bull?
- Important Discovery Exposes Autoimmune Nature of ME/CFS - HERVs Implicated
- The De Meirleir Experience
IMAGES
- Joppe W.R. Hovius, et al. Tick–host–pathogen interactions in Lyme borreliosis. 2007.
- Steer AC, et al. The Emergence of Lyme disease. 2004.
- Pachner AR, et al. Lyme neuroborreliosis: infection, immunity, and inflammation. 2007.
- Mayne PJ. Emerging incidence of Lyme borreliosis, babesiosis, bartonellosis, and granulocytic ehrlichiosis in Australia. 2011.
- Platonov AE, et al. Humans infected with relapsing fever spirochete Borrelia miyamotoi , Russia. 2011.
- Frazer, et al. Genomic sequence of a Lyme disease spirochaete, Borrelia burgdorferi. 1997.
- Elizabeth Fuller, et al. β-Lactam Resistance in Staphylococcus aureus Cells That Do Not Require a Cell Wall for Integrity. 2005.
- A Kersten, et al. Effects of penicillin, ceftriaxone, and doxycycline on morphology of Borrelia burgdorferi. 1995.
- Sapi E, et al. Characterization of Biofilm Formation by Borrelia burgdorferi In Vitro. 2012.
- Chan K, et al. Detection of established virulence genes and plasmids to differentiate Borrelia burgdorferi strains. 2012.
- Iceman Autopsy – National Geographic. 2011.
- Kean WF. The musculoskeletal abnormalities of the Similaun Iceman ("ÖTZI"): clues to chronic pain and possible treatments. 2013.
- Aberer E, et al. Molecular mimicry and Lyme borreliosis: a shared antigenic determinant between Borrelia burgdorferi and human tissue. 1989.
- Elizabeth S. Raveche, et al. Evidence of Borrelia Autoimmunity-Induced Component of Lyme Carditis and Arthritis. 2005.
- A M Ercolini, et al. The role of infections in autoimmune disease. 2009.
- John J Halperin et al. Common Misconceptions About Lyme Disease. 14 January 2013.
- van Dop WA, et al. Seronegative lyme neuroborreliosis in a patient using rituximab. 2013.
- Volker von Baehr et al. The Lymphocyte Transformation Test for Borrelia Detects Active Lyme Borreliosis and Verifies Effective Antibiotic Treatment. 2012.
- Raphael B Stricker, et al. Lyme disease: the next decade. 2011.
- Henry M Feder, Jr., et al. A Critical Appraisal of “Chronic Lyme Disease”. 2007.
- Brorson O et al. An in vitro study of the susceptibility of mobile and cystic forms of Borrelia burgdorferi to metronidazole. 1999.
- Gustaw K. Chronic fatigue syndrome following tick-borne diseases. 2003.
- Wormser GP, et al. Implications fo gender in chronic Lyme disease. 2009.
- Steven E Schutzer, et al. Distinct Cerebrospinal Fluid Proteomes Differentiate Post-Treatment Lyme Disease from Chronic Fatigue Syndrome. 2011.
- Mursic VP, et al. Formation and cultivation of Borrelia burgdorferi spheroplast-L-form variants. 1996.
Figures B and H originally published by BioMed Central. Journal of Neuroinflammation. Judith Miklossy, et al. 25 Sep 2008. Persisting atypical and cystic forms of Borrelia burgdorferi and local inflammation in Lyme neuroborreliosis.
B. Dark field microscopy of Borrelia burgdorferi showing the usual spiral form of spirochetes and their agglomeration into colony-like masses.
H. Cystic form of Borrelia burgdoferi spirochetes, entirely covered by a thickened membrane masking the contents of the cyst.
FURTHER READING:
- A History of Cell Wall Deficient Bacteria: A Selection of Researchers Who Have Worked with the L-form.
- Vaccination against Lyme disease: past, present, and future. 2013.
- FDA recorded webinar on Lyme disease diagnostic research. 2012.

