Why dont the CAA use the following in their CME
Two hypotheses have been presented as underlying the CBT model of chronic fatigue syndrome (105). The first hypothesis "assumes that the pathophysiology of CFS is largely irreversible, but considers that a fine-tuning of the patient's understanding and coping behavior may achieve some improvement in his or her quality of life." The second hypothesis is based on the premise that the patient's impairments are learned due to wrong thinking, and "considers the pathophysiology of CFS to be entirely reversible and perpetuated only by the interaction of cognition, behavior, and emotional processes. According to this model, CBT should not only improve the quality of the patient's life, but could be potentially curative" (105). Some proponents suggest that "ideally general practitioners should diagnose CFS and refer patients to a psychotherapist for CBT without detours to medical specialists as in other functional somatic syndromes" (106,107).
The first hypothesis seems reasonable within the multi causal biopsychosocial model of disease and illness, however a cure may be found. But there is much that is objectionable in the very value-laden second hypothesis, with its implied primary causal role of cognitive, behavioral and emotional processes in the genesis of ME/CFS. This hypothesis is far from being confirmed, either on the basis of research findings or from its empirical results. Nevertheless, the assumption of its truth by some has been used to influence attitudes and decisions within the medical community and the general cultural and social milieu of ME/CFS. To ignore the demonstrated biological pathology of this illness, to disregard the patient's autonomy and experience and tell them to ignore their symptoms, all too often leads to blaming patients for their illness and withholding medical support and treatment.
It is unlikely that the CBT and GET studies that were included in the recent review of treatments (108) dealt with comparable homogeneous groups since different inclusion and exclusion criteria were used in selecting the test patients and control groups. For example, in the Prins et al. (106) CBT study on ME/CFS, patients had to meet the CDC criteria "with the exception of the criterion requiring four of eight additional symptoms to be present." If the sole CDC criterion that patients had to meet was prolonged fatigue, is not this study on chronic fatigue, rather than ME/CFS? In a study by Fulcher and White (109), comparing graded aerobic exercise to flexibility therapy, ME/CFS patients who had an appreciable sleep disturbance were excluded because of the effect that poor sleep has on fatigue. This is puzzling as in a study of symptom prevalence and severity by De Becker et al. (45), 94.8% of 951 patients meeting the Holmes criteria, and 91.9% of 1,578 patients meeting the Fukuda criteria, reported sleep disturbance with an average severity of 2.5 and 2.4, respectively, out of 3. When sleep disturbance is such an integral part of ME/CFS, do the findings in the Fulcher and White study (109) apply to ME/CFS?
A systematic review of prognosis studies show that the less stringent the clinical criteria, the better the prognosis (74). In two of the studies reviewed (110,37), 22% and 26% of patients with chronic fatigue reported recovery, respectively, whereas none and 6% of the ME/CFS patients recovered from fatigue. Therefore, care must be taken not to classify patients experiencing chronic fatigue as ME/CFS patients unless they meet all the criteria for ME/CFS, as the outcomes for these two patient groups are substantially different. It is interesting to note that in the treatment review (108), all the CBT and GET studies that indicated improvement used the less restrictive Oxford criteria with the exception of the Prins study (106) that used the CDC criteria for prolonged fatigue but eliminated the other CDC criteria. All studies excluded ME/CFS patients who were too ill to regularly attend treatment sessions.
The complexity of CBT studies, their varied inclusion and exclusion criteria, the very limited portions that can be properly blinded, and the subjective means used for most evaluations, puts in question the validity of their results. In addition, the numerous variables between the CBT studies, the CBTs and control programs, the different comparison therapies, and the varied frequency and duration of therapy, make it very challenging to determine which parts are responsible for any perceived improvement. Are any effects due to the shift in cognitive beliefs, the exercise involved, the amount and quality of the attention and counseling, the discontinuance of other medical therapies during the test period, etc.? Thus the Powell et al. study (111) found GET alone to be as effective as CBT, and the Risdale et al. study (112) found CBT to be no more effective than counseling.
The GETs included in the review (108) generally involved graded aerobic activities with variable amounts of supervision. These three studies (109,111,113) showed positive effects but the results were modest. Although the more carefully supervised study of Fulcher and White (109) found that 55% of the patients improved over a three month period compared to 27% of patients given flexibility and relaxation exercises, the most common result in both groups was "feeling a little better." Since "graded aerobic exercises programs can help reduce incapacity and symptoms in many chronic and painful conditions" (109), one wonders about the specificity of any effects in ME/CFS patients.
Do study results represent a true reflection of the ME/CFS population when there is a high dropout rate? The Prins et al. study (106) on CBT reported significant improvement in fatigue severity in 35% (20 of 58) of the patients. However, these figures do not reflect that 26% (99 of 377) of the patients who were eligible for the study "refused to take part," and of the 93 patients who were assigned to CBT, 41% (38) did not complete the trial. In a British study (100), 1,214 of 2,338 patients had tried graded exercise. Of these 417 found it to be helpful, 197 reported no change and 610 (50%) indicated that it made their condition worse. This was the highest negative rating of any of the pharmacological, non-pharmacological and alternate approaches of management covered in the questionnaire and may help explain the high drop out rates noted in some of these programs.
The question arises whether a formal CBT or GET program adds anything to what is available in the ordinary medical setting. A well informed physician empowers the patient by respecting their experiences, counsels the patients in coping strategies, and helps them achieve optimal exercise and activity levels within their limits in a common sense, non-ideological manner, which is not tied to deadlines or other hidden agenda.
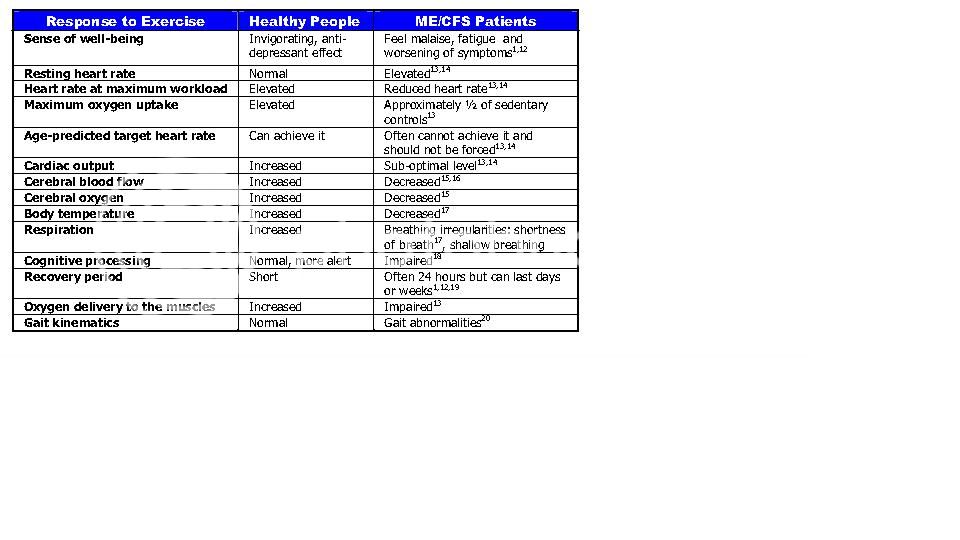
Physicians must take as much care in prescribing appropriate exercise as in prescribing medications to ME/CFS patients (100). Attending physicians should only approve of exercise programs in which the patient's autonomy is respected, appropriate pacing is encouraged, fluctuations in severity of symptoms are taken into account, and adequate rest periods are incorporated. Patients should be monitored frequently but unobtrusively for signs of relapse.