-

Welcome to Phoenix Rising!
Created in 2008, Phoenix Rising is the largest and oldest forum dedicated to furthering the understanding of, and finding treatments for, complex chronic illnesses such as chronic fatigue syndrome (ME/CFS), fibromyalgia, long COVID, postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), and allied diseases.
To become a member, simply click the Register button at the top right.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Article: Coalition4ME/CFS Puts Out Call For Action on DSM-5 Proposal
- Thread starter Phoenix Rising Team
- Start date
Good point Lynn. I will provide examples of letters that orgs have sent out. Thanks to MEAgenda for providing links to them on her website.
COALITION LETTER
COALITION LETTER
[FONT=Helvetica, Arial, sans-serif]To: [/FONT][FONT=Helvetica, Arial, sans-serif]The DSM-5 Task Force and the Somatic Symptom Disorders Work Group
[/FONT]
[FONT=Helvetica, Arial, sans-serif]From:[/FONT][FONT=Helvetica, Arial, sans-serif] Coalition 4 ME/CFS
[/FONT]
[FONT=Helvetica, Arial, sans-serif]Subject:[/FONT][FONT=Helvetica, Arial, sans-serif] Response on the Proposal for Complex Somatic Symptom Disorders and Simple Somatic
[/FONT]
[FONT=Helvetica, Arial, sans-serif] Symptom DIsorders
[/FONT]
[FONT=Helvetica, Arial, sans-serif]Date:[/FONT][FONT=Helvetica, Arial, sans-serif] June 2, 2011[/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
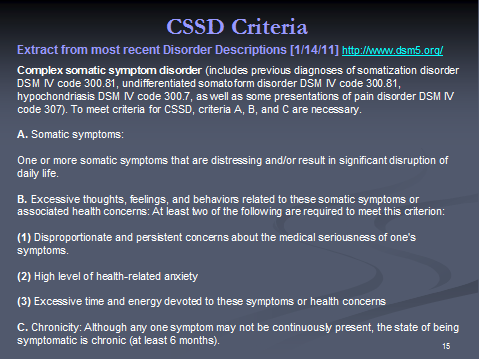
[FONT=Helvetica, Arial, sans-serif]As the Coalition 4 ME/CFS, we wish to comment on the proposals for DSM-5 and particularly on the newly created category for "Complex Somatic Symptom Disorder" (CSSD) and the category Simple Somatic Symptom Disorder (SSSD). [/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]We are very concerned about the real harm that can come to patients through the misuse of the SSD and especially the CSSD in clinical practice. This is especially true for patients with ME/CFS or other diseases like Fibromyalgia, Gulf War Illness and IBS that are misunderstood, misdiagnosed and mistreated by the medical community at large. And while the DSM-5 proposal itself does not call out any specific disease, there is additional concern for ME/CFS patients because of discussions over time that have mentioned CFS specifically in the context of somatic presentations of mental disorders (4).[/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]The biggest concerns are:
[/FONT]
[FONT=Helvetica, Arial, sans-serif]1.Continued stigma for ME/CFS: Despite ample evidence of the pathobiology of ME/CFS (5), patients are still subject today to the insistence by their doctors that there is nothing wrong and they are just depressed. Establishing the CSSD framework that includes hypochondriacs and yet could also be easily applied to patients with real and serious medical diseases like ME/CFS only exacerbates the stigma and mistreatment that these patients have suffered for years. ME/CFS is especially subject to this because the ICD-10-CM categorizes CFS under Signs and Symptoms/Malaise and Fatigue and because those studying somatic symptoms of mental disorders specifically call out CFS (4). [/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]2.Misuse and misapplication of the category: The highly subjective nature of the criteria, especially when applied to real diseases that are poorly understood by the practicing physicians, will lead to misuse of this category and the incorrect diagnosis of a psychological disorder. The Justification for Criteria Somatic Symptoms (3) acknowledges that A key issue is whether the guidelines for CSSD describe a valid construct and can be used reliably. Unfortunately, the document does not provide a satisfactory explanation. There are severity metrics proposed for CSSD but these do little to allay concerns when the benchmarks for normal response include healthy volunteers on the one hand and hypochondriacs on the other. How will these instruments be validated for ME/CFS, which has recently been reported to have a greater impact on functional status and well being than other chronic diseases such as cancer (6)? [/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]This is a huge issue for patients with diseases that are poorly understood. Every day, people who are very sick with real diseases like ME/CFS, Lyme disease, Fibromyalgia, Gulf War Illness and IBS are told that there is nothing wrong with them. It is not hard to imagine that their unwillingness to accept that diagnosis could be judged as disproportionate and persistent concerns about the medical seriousness of one's symptoms by their medical doctors. Once the physician applies a mental health label by diagnosing CSSD (whether as the primary diagnosis or as a secondary diagnosis), there will be profound implications for the patient for diagnosis, treatment, disability and insurance.
[/FONT]
[FONT=Helvetica, Arial, sans-serif]3.Inappropriate Treatments and Withholding of Needed Diagnostics: The Justification for Criteria Somatic Symptoms (3), in explaining the creation of CSSD, states that treatment interventions are similar in this group of disorders and describes the use of antidepressant medications and CBT for the identification and modification of dysfunctional and maladaptive beliefs about symptoms and disease, and behavioral techniques to alter illness and sick role behaviors and promote more effective coping. It further states that all of these disorders benefit from specific interventions with the patients non-psychiatric physician (e.g. scheduling regular appointments as opposed to prn appointments, limiting testing and procedures unless clearly indicated). We only need to look to England and the NICE Guidelines to understand the disastrous effects of such standards. In the hands of a doctor truly knowledgeable about ME/CFS, CBT and anti-depressants may sometimes be part of an effective treatment plan. But all too often, the treatments are misused by doctors who dont understand the disease and instead believe that the real problem with the patient is his false illness beliefs or that he is just depressed. Suggesting that doctors focus on these as treatments and limit testing and procedures in such a scenario could have a disastrous impact on the patients life.
[/FONT]
[FONT=Helvetica, Arial, sans-serif]4.Alignment with ICD: While the DSM-5 is separate from the ICD-10 and is used primarily by mental health practitioners, there is an alignment between the two today. It appears that that will continue with ICD-11 although it is not clear at this time how that will be achieved. Instituting the CSSD in the ICD-11 would have negative implications not only for the US but also for all other countries.
[/FONT]
[FONT=Helvetica, Arial, sans-serif]We are not alone in voicing serious concern for the unintended consequences of the DSM-5 plans for SSSD and CSSD. Numerous organizations and individuals stated these same concerns in the April 2010 review cycle yet the CSSD category remains essentially unchanged. Even members of the psychiatric community, most prominently Dr. Allen Frances, the chair of the DSM-IV task force and Dr. Robert Spitzer, the chair of the DSM-III task force, have raised concerns with the process, content, direction and unintended consequences of the DSM-5 (7,8,9). Dr. Allen Frances (the chair of the DSM-IV task force) raised this issue of the unintended consequences of the DSM-5, especially around a premature paradigm shift. In A Warning Sign on the Road to DSM-5: Beware of Its Unintended Consequences (7), he states Part of the exaggerated claim of a paradigm shift in DSM-5 is based on the suggestion that it will be introducing dimensional ratings and that this will increase the precision of diagnosis [But] Including an ad hoc, untested, and complex dimensional system in an official nomenclature is premature and will likely lead to similar neglect and confusion.
[/FONT]
[FONT=Helvetica, Arial, sans-serif]We urge you to seriously reconsider the inclusion of this category. For ME/CFS patients and for many other patients with other real but poorly understood diseases, those unintended consequences of implementing CSSD and SSSD could be disastrous![/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]Thank you.
[/FONT]
[FONT=Helvetica, Arial, sans-serif]Coalition 4 ME/CFS
[/FONT]
[FONT=Helvetica, Arial, sans-serif]References
[/FONT]
[FONT=Helvetica, Arial, sans-serif]1) Somatic Symptom Disorders, DSM website, May 29, 2011, ([/FONT][FONT=Helvetica, Arial, sans-serif]http://www.dsm5.org/ProposedRevision/Pages/SomaticSymptomDisorders.aspx[/FONT][FONT=Helvetica, Arial, sans-serif]) [/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]2) Somatic Symptom Disorders, description published by the American Psychiatric Association, Draft 4/18/2011, ([/FONT][FONT=Helvetica, Arial, sans-serif]www.dsm5.org/Documents/Somatic/Somatic%20Symptom%20Disorders%20description%20April%2018,%202011.pdf[/FONT][FONT=Helvetica, Arial, sans-serif]) [/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]3) Justification for Criteria Somatic Symptoms, Published by the American Psychiatric Association, Draft 4/18/2011, ([/FONT][FONT=Helvetica, Arial, sans-serif]www.dsm5.org/Documents/Somatic/DSM Validity Propositions 4-18-11.pdf[/FONT][FONT=Helvetica, Arial, sans-serif])
[/FONT]
[FONT=Helvetica, Arial, sans-serif]4) Michael First for the American Psychiatric Institute, Somatic Presentations of Mental Disorders (September 6-8, 2006), ([/FONT][FONT=Helvetica, Arial, sans-serif]http://www.dsm5.org/research/pages/somaticpresentationsofmentaldisorders(september6-8,2006).aspx[/FONT][FONT=Helvetica, Arial, sans-serif]) [/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]5) NIH State of Knowledge Workshop on ME/CFS Video and agenda, April 7-8, 2011 ([/FONT][FONT=Helvetica, Arial, sans-serif]http://orwh.od.nih.gov/CSF 2011/newsEvents.htm[/FONT][FONT=Helvetica, Arial, sans-serif])
[/FONT]
[FONT=Helvetica, Arial, sans-serif]6) L. Nacul et al., The functional status and well being of people with myalgic encephalomyelitis/chronic fatigue syndrome and their carers, BMC Public Heath, May 27, 2011 [/FONT][FONT=Helvetica, Arial, sans-serif](http://www.biomedcentral.com/1471-2458/11/402/abstract[/FONT][FONT=Helvetica, Arial, sans-serif])[/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]7) Dr. Allen Frances, MD, A Warning Sign on the Road to DSM-5: Beware of Its Unintended Consequences, Psychiatric Times. June 26, 2009. ([/FONT][FONT=Helvetica, Arial, sans-serif]http://www.psychiatrictimes.com/dsm-5/content/article/10168/1425378[/FONT][FONT=Helvetica, Arial, sans-serif])
[/FONT]
[FONT=Helvetica, Arial, sans-serif]8) Dr. Allen Frances (DSM IV) and Dr. Robert Spitzer (DSM-III), Letter to the APA board of trustees. July 6, 2009. ([/FONT][FONT=Helvetica, Arial, sans-serif]http://www.scribd.com/doc/17172432/...-7-2009-From-Allen-Frances-and-Robert-Spitzer[/FONT][FONT=Helvetica, Arial, sans-serif]) [/FONT][FONT=Helvetica, Arial, sans-serif]
[/FONT]
[FONT=Helvetica, Arial, sans-serif]9) Gary Greenberg, Inside the battle to define Mental Illness, Wired Magazine. Dec 27, 2010. ([/FONT][FONT=Helvetica, Arial, sans-serif]http://www.wired.com/magazine/2010/12/ff_dsmv/all/1[/FONT][FONT=Helvetica, Arial, sans-serif])[/FONT]
The CFIDS Association of America Response http://www.cfids.org/advocacy/2010/dsm5-statement.pdf
April 1, 2010
DSM-5 Task Force
American Psychiatric Association
1000 Wilson Boulevard Suite 1825 Arlington, VA 22209
Members of the DSM-5 Task Force,
In response to an open request for input on proposed changes to the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM), the CFIDS Association of America submits the following statement and urgent recommendation.
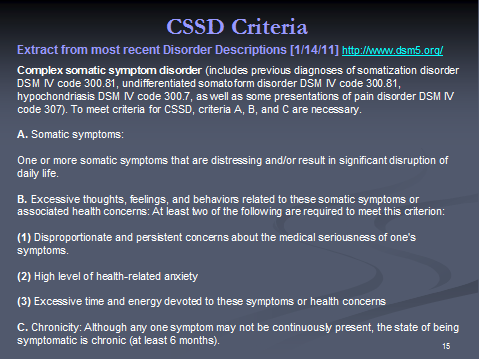
The CFIDS Association strongly questions the utility of the proposed rubric of complex somatic symptom disorder (CSSD). According to the DSM-5 website (http://www.dsm5.org/Documents/Somatic/APA Somatic Symptom Disorders description January29 2010.pdf, accessed March 28, 2010):
To meet criteria for CSSD, criteria A, B, and C are necessary.
A. Somatic symptoms:
Multiple somatic symptoms that are distressing, or one severe symptom
B. Misattributions, excessive concern or preoccupation with symptoms and illness: At least two of the following are required to meet this criterion:
(1) High level of health-related anxiety.
(2) Normal bodily symptoms are viewed as threatening and harmful
(3) A tendency to assume the worst about their health (catastrophizing).
(4) Belief in the medical seriousness of their symptoms despite evidence to the contrary.
(5) Health concerns assume a central role in their lives
C. Chronicity: Although any one symptom may not be continuously present, the state of being symptomatic is chronic and persistent (at least six months).
The creation of CSSD appears to violate the charges to DSM-5 Work Groups to clarify boundaries between mental disorders, other disorders and normal psychological functioning (http://www.dsm5.org/about/Pages/faq.aspx, accessed March 28, 2010). This is especially true with regard to patients coping with conditions characterized by unexplained medical symptoms, or individuals with medical conditions that presently lack a mature clinical testing regimen that provides the evidence required to substantiate the medical seriousness of their symptoms.
For instance, all of the case definitions for CFS published since 1988 have required that in order to be classified/diagnosed as CFS, symptoms must produce substantial impact on the patients ability to engage in previous levels of occupational, educational, personal, social or leisure activity. Yet, all of the case definitions rely on patient report as evidence of the disabling nature of symptoms, rather than results of specific medical tests. So by definition, CFS patients will meet the CSSD criteria A and C for somatic symptoms and chronicity, and by virtue of the lack of widely available objective clinical tests sensitive and specific to its characteristic symptoms, CFS patients may also meet criterion B-4.
As drafted, the criteria for CSSD establish a Catch-22 paradox in which six months or more of a single or multiple somatic symptoms surely a distressing situation for a previously active individual is classified as a mental disorder if the individual becomes excessively concerned about his or her health. Without establishing what normal behavior in response to the sustained loss of physical health and function would be and in the absence of an objective measure of what would constitute
excessiveness, the creation of this category poses almost certain risk to patients without providing any offsetting improvement in diagnostic clarity or targeted treatment.
To provide another common example, back pain that is debilitating and severe, with negative MRIs, is still debilitating and severe back pain. A patient in this situation might be concerned about this back pain, might view it as detrimental to his quality of life and livelihood, and might direct time and resources to seeking care from multiple specialists (e.g., neurology, rheumatology, orthopedics, rehabilitation) to relieve it.
Each of these specialists is likely to recommend slightly different therapies, compounding the patients focus on alternative explanations for and long-term impact of decreased function and diminished health. Such a patient could be diagnosed with CSSD, yet no empiric evidence has been provided by the Somatic Symptoms Disorders Work Group that applying the label of CSSD will facilitate communication
with the patient, add clinical value to the patients experience, or improve the care any of these various specialists might provide.
The Somatic Symptoms Disorder Work Group states that patients fitting these criteria are generally encountered in general medical settings, rather than mental health settings (http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=368#, accessed March 28, 2010), further limiting the usefulness of this classification in a manual written primarily for the benefit of mental health professionals.
The Somatic Symptoms Disorders Work Group conveys considerable uncertainty about the impact of this new label, in spite of the charge to all DSM-5 work groups to demonstrate the strength of research for the recommendations on as many evidence levels as possible. The Somatic Symptoms Disorders Work Group states:
It is unclear how these changes would affect the base rate of disorders now recognized as somatoform disorders. One might conclude that the rate of diagnosis of CSSD would fall, particularly if some disorders previously diagnosed as somatoform were now diagnosed elsewhere (such as adjustment 2disorder). On the other hand, there are also considerable data to suggest that physicians actively avoid using the older diagnoses because they find them confusing or pejorative. So, with the CSSD classification, there may be an increase in diagnosis. (http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=368#, accessed March 28, 2010)
The proposed DSM-5 revision correctly does not identify chronic fatigue syndrome (CFS) as a condition within the domain of mental disorders and the DSM. However, past discussions of the Somatic Symptoms Disorder Work Group have included such physiological disorders as chronic fatigue syndrome, irritable bowel syndrome and fibromyalgia (http://www.dsm5.org/Research/Pages/SomaticPresentationsofMentalDisorders(September6-8,2006).aspx) as somatic presentations of mental disorders. None of the research and/or clinical criteria for chronic fatigue syndrome published since 1988 have established CFS as a mental disorder and a continuously growing body of literature demonstrates CFS to be a physiological disorder marked by abnormalities in the central and autonomic nervous systems, the immune system and the endocrine system. The role of infectious agents in the onset and/or persistence of CFS has received renewed attention since the DSM-5 revision process began in 1999. Most recently, the October 2009 report of evidence of a human retrovirus, xenotropic murine leukemia-related retrovirus (XMRV), in CFS patients in Science (Lombardi, 2009) has generated new investigations into this and other infectious agents in CFS.
The conceptual framework for CFS detailed in the Clinical Working Case Definition, Diagnostic and Treatment Protocols (Carruthers, 2003) serves as a useful tool for professionals to establish a diagnosis of CFS, address comorbidities that may complicate the clinical presentation and distinguish CFS from conditions with overlapping symptomotology. Research on CFS continues to explore and document important biomarkers. Lack of known causation does not make CFS or the CFS patients illness experience psychopathological any more than multiple sclerosis, diabetes, or other chronic illnesses with objective diagnostic measures, would be so considered.
For the reasons stated above and the general failure of the proposed creation of the CSSD to satisfy the stated objectives of the DSM-5 without risking increased harm to patients through confusion with other conditions or attaching further stigma, the CFIDS Association strongly urges the DSM-5 Task Force to abandon the proposed creation of CSSD.
Sincerely,
K.
Mass CFIDS/ME Association Response
The Massachusetts CFIDS/ME & FM Association has joined with other U.S. patient organizations to advocate against the potential misuse of a proposed new psychiatric diagnostic category in the diagnosis of CFIDS/ME and Fibromyalgia.
The revision of the current Diagnostic and Statistical Manual of Mental Disorders - Fourth Edition (DSM-IV ) is at the core of our concerns. This Manual, published by the American Psychiatric Association (APA), contains the major listings, definitions, and explanations of different psychiatric and psychological disorders. It is important to note these classifications are used by insurance companies, Medicaid and Medicare for patient billing purposes.
Currently DSM-IV is undergoing a major revision - the new DSM-V Manual is scheduled to be published in 2013. The issue which has raised the serious concern of both U.S. patient associations and of the international CFIDS/ME researchers (the International Association of CFS/ME - IACFS-ME) is a proposed new psychiatric category titled the:Complex Somatic Symptom Disorder (CSSD) to be included in the new DSM-V.
More specifically, the way CSSD is defined makes it possible to either mistakenly or intentionally diagnose CFIDS/ME or Fibromyalgia in this psychiatric category. Moreover, the greater concern is whether this change could potentially lead to the reclassification of these illnesses as psychiatric conditions under CSSD.
The crux of the issue is that a person can be psychiatrically diagnosed as having complex somatic symptom disorder if he or she has all of the following:
a) multiple somatic (physical) symptoms, or one severe symptom that have been chronic fatigue for at least six months, and
b) which create a high level of health anxiety and which establish a central role in the patient's life for health concerns.
Does this diagnosis sound like it could easily be misused to diagnose CFIDS/ME, fibromyalgia, or even many other chronic physical illnesses? U.S. patients have already experienced the problematic history of The Centers of Disease Control and Prevention (CDC), The National Institutes of Health (NIH), and the many physicians and researchers discounting CFIDS/ME as a psychiatric illness, maladaptive behavior, or inability to cope with stress. If this new diagnostic code were to be accepted, then patients potentially could be labeled with complex somatic symptom disorder just because they are pushing doctors for answers to many symptoms.
In their explanation of the CSSD diagnosis, the American Psychiatric Association (APA) Committee states: "Some patients, for instance, with irritable bowel syndrome or fibromyalgia would not necessarily qualify for a somatic symptom disorder diagnosis."
As a result, this development galvanized patient associations around the country, as well as the IACFS/ME, to protest any misuse of the new CSSD category. This was accomplished by submitting strong letters on behalf of the illnesses to the APA during the comment period, which closed on April 20, 2010.
On behalf of the Massachusetts CFIDS/ME & FM Association and the community it serves, several poignant letters were written to the APA. The first letter was submitted by Dr. Alan Gurwitt, MASS CFIDS/ME & FM Association's President. It focused particularly on the incontrovertible medical research clearly demonstrating the biological and physiological bases of the illnesses. A second letter was submitted by Ken Casanova, a Board member and past President. It reviewed in detail how the new CSSD diagnosis would make it more difficult to separate physical from psychiatric illnesses, and how the new diagnosis could be mistakenly or intentionally misused.
The International Classification of Diseases-Clinical Modification 9 (ICD-CM-9) used by the CDC is different than the version used by WHO. The CDC is planning to update the ICD-CM- 9 to the ICD-CM-10 in 2013. However, the International WHO Code is being updated to version ICD-11 in 2014. This means the code the CDC will be using is still behind the WHO. The CFIDS and FM communities' concern is that the new CSSD classification could influence how CFIDS/ME and FM are listed in both the CDC and WHO classifications.
20+ years after first naming the illness Chronic Fatigue Syndrome, the CDC is now wanting to update its classification. The serious concern is that the new CSDD diagnosis could negatively influence any new CDC listing of CFIDS/ME. Any new psychiatric bias toward CFIDS/ME and/or FM in the new code could make it more difficult for patients to obtain insurance payments for their treatments. There is also, of course, concern about the effect of CSSD on the WHO code.
There is strength in numbers and our organization advocates on behalf of patients and the impact these illnesses have on their lives. Consider joining our Association so that together our voice and our actions will be stronger.
Dr. Alan Gurwitt - Former Psychiatrist and Pres of Mass CFIDS
<table class="contentpaneopen"><tbody><tr><td class="contentheading" width="100%">
</td><td class="buttonheading" width="100%" align="right">
</td><td class="buttonheading" width="100%" align="right">
</td></tr></tbody></table>
<table class="contentpaneopen"><tbody><tr><td class="contentheading" width="100%">
</td><td class="buttonheading" width="100%" align="right"><table class="contentpaneopen"><tbody><tr><td class="contentheading" width="100%">Dr. Alan Gurwitt's letter to DSM-V Committee of the APA
</td><td class="buttonheading" width="100%" align="right">
</td><td class="buttonheading" width="100%" align="right">
</td><td class="buttonheading" width="100%" align="right">
</td></tr> </tbody></table> The Board of Directors of the Massachusetts Chronic Fatigue and Immune Dysfunction Syndrome/Myalgic Encephalopathy and Fibromyalgia Association (Mass. CFIDS/ME &FM) has reviewed your proposed revisions of DSM-IV destined for DSM-V. Our particular focus has been on your newly proposed category "Complex Somatic Symptom Disorder". Our concern is not so much about the fact that you wanted to simplify terms for somatoform disorders but about the criteria cited and the potential misuse of the category.
We share the concern, heard from individuals and organizations around the world, that this new category might be too readily used to include chronic fatigue syndrome ("CFS", also now known as ME or myalgic encephalopathy) and fibromyalgia as if they are forms of a psychological disorder. Most simply, they are not now psychologically caused illnesses nor have they ever been so. This concern doesn't come out of the blue. It is based on two and a half decades of mistaken and harmful misdiagnoses based on totally inappropriate and harmful misconceptions of what CFS and fibromyalgia are and what they are caused by.
Our organization, celebrating our 25th year of existence helping patients with these illnesses, has seen firsthand the terrible toll exacted by the trail of misdiagnoses. Patients are tainted, dismissed, not properly treated, and often referred to equally misinformed mental health clinicians.
In our view, the key problem is not so much the diagnostic nomenclature as it is the very wrong conceptions on the part of psychiatrists and non-psychiatric physicians of the very nature and likely causes of both CFS/ME and FM. There may be psychological disturbances following the onset; these are important but they are secondary.
Over the past fifteen years, increasing numbers of researchers from around the world have pinpointed the likely biological causes, the complex pathophysiology that follow from the initial infectious or toxic triggers, and the interacting and dysfunctional multiple body systems (immune, central and peripheral nervous systems, endocrine, cellular [mitochondrial], etc) involved. Genetic and genomic factors are being elucidated. Certain viruses have long been implicated. Most recently a retrovirus, XMRV, has been implicated and is actively being studied in several centers. While no widely accepted biomarkers are currently available, many key researchers believe that it will not be long before one or more biomarkers will be found. While there is no definitive cure as yet, forms of treatment have been developed over the years that can alleviate many of the symptoms. Here is where mental health clinicians can help; if there are serious secondary psychological symptoms, certain therapies can help.
Dr. Anthony Komaroff, Professor of Medicine at Harvard Medical School and a long-time researcher in the field has said the following:
"...there are now over 4,000 published studies that show underlying biomedical abnormalities in patients with this illness. It's not an illness that people can simply imagine that they have and it s not a psychological illness. In my view, that debate, which has waged for twenty years, should now be over". Four years later there is even more evidence for Dr. Komaroff's assertion.
The bottom line is that CFS and fibromyalgia are not psychological illnesses. It is then essential that the American Psychiatric Association vigorously help educate graduate and resident psychiatrists on this essential truth. While the wording and criteria for "Complex Somatic Symptom Disorder" will matter so as to avoid confusing chronic fatigue syndrome and fibromyalgia with a somatoform disorder it will be new understanding of the biological nature, proper diagnostic techniques, and appropriate treatments of these illnesses that will matter most.
Alan Gurwitt, M.D.
President, Massachusetts CFIDS/ME & FM Association
(Retired adult and child psychiatrist, Distinguished Fellow of the American Psychiatric Association)
4/15/10
</td><td class="buttonheading" width="100%" align="right">
</td><td class="buttonheading" width="100%" align="right">
</td></tr></tbody></table>
Readers please note that the CFIDS and MassCFIDS responses that Cort has posted are examples of last year's submissions - not from this year.
There is a new page opened on my site for this year's responses. It is currently empty.
2010 submissions: http://wp.me/PKrrB-AQ
2011 submissions: http://wp.me/PKrrB-19a
UK org, Action for M.E., confirmed yesterday that they are intending to submit again, this year, but as yet, no other UK orgs have confirmed.
Have you found PR's response from last year, yet, Cort? I would be happy to add it to the others on my site.
I am pleased to see that this coaliton of 8 US orgs has now put out a "Call to Action", but it is a pity that this could not have been issued earlier.
My alert and call for action for the second public review period was posted here, on Co-Cure and on my site on 5 May.
There are now only 13 days left.
Why is the American Psychiatric Association referred to in the Coalition4ME/CFS's materials as the "ASA"?
I have copies of last year's submissions on my site for:
International patient organisation submissions:
Whittemore Peterson Institute, Steungroep CFS Netherlands, CFS Associazione Italiana, ME Association (endorsed submission of Dr E Goudsmit), Action for M.E., Invest in ME, Mass. CFIDS/ME & FM, The CFIDS Association of America, Vermont CFIDS Association, IACFSME, The 25% ME Group
Patient advocate submissions:
Suzy Chapman UK (2), Tammie Page M.A. US, Patient advocate US, John Mizelle, Therapist US, Peter Kemp UK, Ian McLachlan UK, Andrew US, Mary M. Schweitzer PhD US
Suzy Chapman
me.agenda@virgin.net
http://dxrevisionwatch.wordpress.com
http://meagenda.wordpress.com
There is a new page opened on my site for this year's responses. It is currently empty.
2010 submissions: http://wp.me/PKrrB-AQ
2011 submissions: http://wp.me/PKrrB-19a
UK org, Action for M.E., confirmed yesterday that they are intending to submit again, this year, but as yet, no other UK orgs have confirmed.
Have you found PR's response from last year, yet, Cort? I would be happy to add it to the others on my site.
I am pleased to see that this coaliton of 8 US orgs has now put out a "Call to Action", but it is a pity that this could not have been issued earlier.
My alert and call for action for the second public review period was posted here, on Co-Cure and on my site on 5 May.
There are now only 13 days left.
Why is the American Psychiatric Association referred to in the Coalition4ME/CFS's materials as the "ASA"?
I have copies of last year's submissions on my site for:
International patient organisation submissions:
Whittemore Peterson Institute, Steungroep CFS Netherlands, CFS Associazione Italiana, ME Association (endorsed submission of Dr E Goudsmit), Action for M.E., Invest in ME, Mass. CFIDS/ME & FM, The CFIDS Association of America, Vermont CFIDS Association, IACFSME, The 25% ME Group
Patient advocate submissions:
Suzy Chapman UK (2), Tammie Page M.A. US, Patient advocate US, John Mizelle, Therapist US, Peter Kemp UK, Ian McLachlan UK, Andrew US, Mary M. Schweitzer PhD US
Suzy Chapman
me.agenda@virgin.net
http://dxrevisionwatch.wordpress.com
http://meagenda.wordpress.com
Should we try to get some Doctors who specialize in ME/CFS to write letters to them too?
I would think that along with all these organizations, coalitions and patients letters, the voice of MDs could add more credence.
Do you think, in addition that a petition-like letter signed by many patients would help. I would think that it might take too much energy for some patients to do this on their own but if all they have to do is sign it, it would make it much easier for them.
Thanks for doing this Cort. I think that this is major!.
Nielk
I would think that along with all these organizations, coalitions and patients letters, the voice of MDs could add more credence.
Do you think, in addition that a petition-like letter signed by many patients would help. I would think that it might take too much energy for some patients to do this on their own but if all they have to do is sign it, it would make it much easier for them.
Thanks for doing this Cort. I think that this is major!.
Nielk
Should we try to get some Doctors who specialize in ME/CFS to write letters to them too?
I would think that along with all these organizations, coalitions and patients letters, the voice of MDs could add more credence.
Do you think, in addition that a petition-like letter signed by many patients would help. I would think that it might take too much energy for some patients to do this on their own but if all they have to do is sign it, it would make it much easier for them.
Thanks for doing this Cort. I think that this is major!.
Nielk
No, I don't think petitions would be acceptable to the APA. The process for submitting responses is via individuals registering on the DSM-5 Development site to upload an individual comment.
APA DSM5 - PANDORA ALSO SUBMITTED INPUT IN 2010
Here is PANDORA 2010 letter to APA on DSM5
In addition through our urging Shelley Foote, a clinical psychologist who is associated with the Dade County Psychological Association (DCPA)...shared with PANDORA last year: "Had our DCPA full-day meeting and I am wiped out but I wanted to tell you, despite missing DSM-5' theoretical deadline, I have over 25 letters signed by psychologists expressing their disagreement and disapproval of the CSSD category.I typed out a letter last night, printed it, gave it to them along with your AWESOME letter and a stamped, addressed envelope, how could they say no, right?Just wanted you to know - now go and enjoy the mountain air!!!"
The Coalition4MECFS Call to Action is part of a series of position statements that this young coalition members will publish and collectively push for an agenda that will benefit the patient community they serve.
Please feel free to use our letter as a sample or template for one of your own.
We are grateful to Mary Dimmock, Michael Munoz & Lori Chapo Kroger for their dedication and commitment to get our first Call to Action in place so quickly and effectively.
Marly Silverman, Founder, PANDORA - Dash to www.p-a-n-d-o-r-a.org
Member, Steering Committee, Coalition4MECFS
PANDORA is a proud Charter Member of the Coalition4MECFS.org
Here is PANDORA 2010 letter to APA on DSM5
In addition through our urging Shelley Foote, a clinical psychologist who is associated with the Dade County Psychological Association (DCPA)...shared with PANDORA last year: "Had our DCPA full-day meeting and I am wiped out but I wanted to tell you, despite missing DSM-5' theoretical deadline, I have over 25 letters signed by psychologists expressing their disagreement and disapproval of the CSSD category.I typed out a letter last night, printed it, gave it to them along with your AWESOME letter and a stamped, addressed envelope, how could they say no, right?Just wanted you to know - now go and enjoy the mountain air!!!"
The Coalition4MECFS Call to Action is part of a series of position statements that this young coalition members will publish and collectively push for an agenda that will benefit the patient community they serve.
Please feel free to use our letter as a sample or template for one of your own.
We are grateful to Mary Dimmock, Michael Munoz & Lori Chapo Kroger for their dedication and commitment to get our first Call to Action in place so quickly and effectively.
Marly Silverman, Founder, PANDORA - Dash to www.p-a-n-d-o-r-a.org
Member, Steering Committee, Coalition4MECFS
PANDORA is a proud Charter Member of the Coalition4MECFS.org
Readers please note that the CFIDS and MassCFIDS responses that Cort has posted are examples of last year's submissions - not from this year.
There is a new page opened on my site for this year's responses. It is currently empty.
2010 submissions: http://wp.me/PKrrB-AQ
2011 submissions: http://wp.me/PKrrB-19a
UK org, Action for M.E., confirmed yesterday that they are intending to submit again, this year, but as yet, no other UK orgs have confirmed.
Have you found PR's response from last year, yet, Cort? I would be happy to add it to the others on my site.
I am pleased to see that this coaliton of 8 US orgs has now put out a "Call to Action", but it is a pity that this could not have been issued earlier.
My alert and call for action for the second public review period was posted here, on Co-Cure and on my site on 5 May.
There are now only 13 days left.
Why is the American Psychiatric Association referred to in the Coalition4ME/CFS's materials as the "ASA"?
I have copies of last year's submissions on my site for:
International patient organisation submissions:
Whittemore Peterson Institute, Steungroep CFS Netherlands, CFS Associazione Italiana, ME Association (endorsed submission of Dr E Goudsmit), Action for M.E., Invest in ME, Mass. CFIDS/ME & FM, The CFIDS Association of America, Vermont CFIDS Association, IACFSME, The 25% ME Group
Patient advocate submissions:
Suzy Chapman UK (2), Tammie Page M.A. US, Patient advocate US, John Mizelle, Therapist US, Peter Kemp UK, Ian McLachlan UK, Andrew US, Mary M. Schweitzer PhD US
Suzy Chapman
me.agenda@virgin.net
http://dxrevisionwatch.wordpress.com
http://meagenda.wordpress.com
I'd like to add a little background information to the Coalition notice paragraph 4:
The striving for "harmonization" between DSM categories and ICD Chapter V (the Mental and behavioural disorders chapter of ICD-10) categories is a process initiated many years ago, during the development of both existing editions.
The APA and the WHO, Geneva, have already achieved a degree of congruency between categories in the existing DSM-IV and categories in Chapter V of ICD-10.
For example, this is a simplified table showing how the "Somatoform Disorders" categories currently compare within the two classification systems.
(The disorder descriptions are not exactly the same, nor are the criteria, but there is a degree of correspondence. Note also that while ICD-10 Chapter V classifies "Neurasthenia", the DSM has dropped "Neurasthenia" for DSM-IV.)
Current DSM-IV Codes and Categories for Somatoform Disorders and their ICD-10 Equivalents:
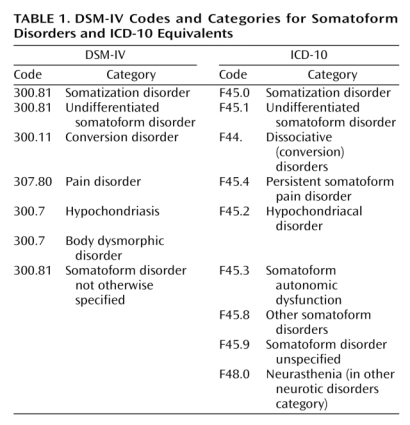
So the process of "harmonization" between DSM-IV and Chapter V of ICD-10 has been a joint undertaking.
The APA participates with the WHO in an "International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders" and the "DSM-ICD Harmonization Coordination Group" which were set up in 2007, and which meet face-to-face a couple of times a year.
The International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders is chaired by DSM-5 Development Task Force member, Dr Steven Hyman, MD and co-ordinated by Dr Geoffrey Reed, PhD, who is seconded to the WHO, Geneva, to co-ordinate the revision of Chapter V (which will be known as Chapter 5 in ICD-11).
For the forthcoming DSM-5 and ICD-11, the APA and the WHO have committed as far as possible:
"To facilitate the achievement of the highest possible extent of uniformity and harmonization between ICD-11 mental and behavioural disorders and DSM-V disorders and their diagnostic criteria."
with the objective that
"The WHO and APA should make all attempts to ensure that in their core versions, the category names, glossary descriptions and criteria are identical for ICD and DSM."
But the WHO acknowledges that there may be sections where congruency between approved DSM-5 categories and the corresponding categories in ICD-11 Chapter 5, may not be achievable.
For example, the WHO has strict taxonomic rules for ICD classifications and codings which will continue to apply to ICD-11 and which may not facilitate the accommodation of the radical overhaul of the "Somatoform Disorders" section that the SSD Work Group is proposing - even if ICD-11 Revision Steering Group and WHO classification experts were to consider these proposals to be valid propositions.
Between one edition and the next, the WHO may, for example, add new disease and disorder terms; or move an existing ICD category term out of the "R code" chapter (Chapter 18) and relocate it in another chapter in response to scientific developments; or move an existing disease or disorder within a chapter to place it under a different parent class; or remove a parent class, as is being proposed for the G93 Other disorders of brain, for ICD-11.
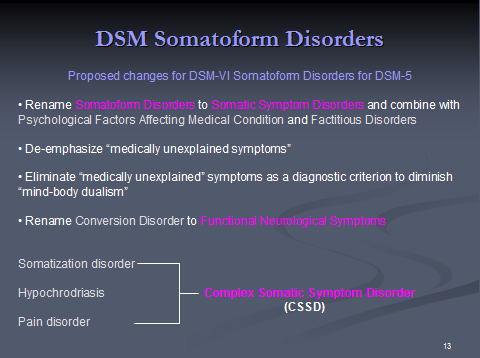
But the SSD Work Group is proposing to take a number of existing categories (which have parallel categories in ICD-10) and combine them under a new category CSSD, thus:
I consider that ICD-11 would find such radical changes difficult to achieve congruency with under ICD taxonomic rules.
So it needs to be understood that the "Somatoform Disorders" (or "Somatic Symptom Disorders", as they propose to rename them) categories for DSM-5 correspond with the "Somatoform Disorders" categories of Chapter 5 Mental and behavioural disorders in the forthcoming ICD-11 - not with Chapter 6 Diseases of the nervous system, where PVFS, (B)ME have been classified since 1992, and to which CFS is indexed.
It's not known to what extent the various DSM-5 Work Groups (there are 13 plus a number of study groups) and the ICD-11 Topic Advisory Group for Mental and behavioural disorders are collaborating or whether the respective sections of DSM-5 and ICD-11 Chapter 5 are being developed in parallel. It's not known either, at what point in the Timelines for the development of both systems, "harmonization" would be anticipated to have been agreed upon, or rejected if not feasible or acceptable to either party for any given section, for whatever reasons.
But the Alpha drafting platform for ICD-11 currently shows no evidence of mirroring the radical proposals that the DSM-5 SSD Work Group are proposing.
ICD-11 is now running around a year behind with its own Beta draft and has just shifted its Beta Timeline by 12 months, so it's running even more out of synch with DSM-5.
DSM-5 will need to be largely completed by March-December 2012 for presentation to the APA Board of Trustees, whereas ICD-11 isn't now expecting to launch its Beta draft until May 2012 - so the slipping Timelines for ICD-11 and the differences between their drafting and field trial schedules may also present barriers to "harmonization".
DSM-5 is also expected to "harmonize" with the forthcoming US specific ICD-10-CM, for which a partial code freeze will be implemented this year, in October 2011. So the drafting schedules for all three systems are no longer in synch.
You can see the ICD-11 Alpha draft page for "Somatoform Disorders" here:
http://apps.who.int/classifications/icd11/browse/l-m/en#/@_@who_3_int_1_icd_2_F45
(You will need to click the drop down for child classes.)
PVFS, (B)ME and CFS in ICD-11:
For ICD-11 Alpha draft, the proposal is for CFS, PVFS and (B)ME to be classified in Chapter 6, with PVFS -> CFS specified as an Exclusion to Chapter 5 "Somatoform Disorders".
See screenshots for ICD-11 Alpha draft for CFS, showing (Benign) ME specified as an Inclusion term to CFS in Chapter 6 Diseases of the nervous system, plus further notes on the proposals for PVFS, CFS and (Benign) ME in this post: http://wp.me/pKrrB-16N
me.agenda@virgin.net
http://dxrevisionwatch.wordpress.com
http://meagenda.wordpress.com
4.Alignment with ICD: While the DSM-5 is separate from the ICD-10 and is used primarily by mental health practitioners, there is an alignment between the two today. It appears that that will continue with ICD-11 although it is not clear at this time how that will be achieved. Instituting the CSSD in the ICD-11 would have negative implications not only for the US but also for all other countries.
The striving for "harmonization" between DSM categories and ICD Chapter V (the Mental and behavioural disorders chapter of ICD-10) categories is a process initiated many years ago, during the development of both existing editions.
The APA and the WHO, Geneva, have already achieved a degree of congruency between categories in the existing DSM-IV and categories in Chapter V of ICD-10.
For example, this is a simplified table showing how the "Somatoform Disorders" categories currently compare within the two classification systems.
(The disorder descriptions are not exactly the same, nor are the criteria, but there is a degree of correspondence. Note also that while ICD-10 Chapter V classifies "Neurasthenia", the DSM has dropped "Neurasthenia" for DSM-IV.)
Current DSM-IV Codes and Categories for Somatoform Disorders and their ICD-10 Equivalents:
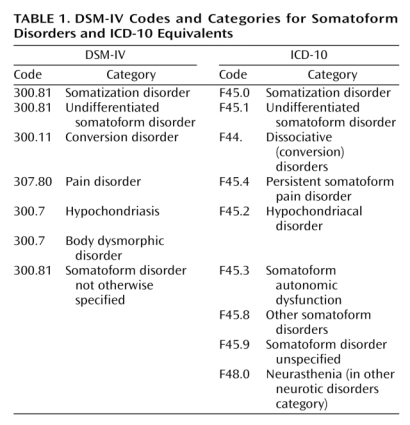
So the process of "harmonization" between DSM-IV and Chapter V of ICD-10 has been a joint undertaking.
The APA participates with the WHO in an "International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders" and the "DSM-ICD Harmonization Coordination Group" which were set up in 2007, and which meet face-to-face a couple of times a year.
The International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders is chaired by DSM-5 Development Task Force member, Dr Steven Hyman, MD and co-ordinated by Dr Geoffrey Reed, PhD, who is seconded to the WHO, Geneva, to co-ordinate the revision of Chapter V (which will be known as Chapter 5 in ICD-11).
For the forthcoming DSM-5 and ICD-11, the APA and the WHO have committed as far as possible:
"To facilitate the achievement of the highest possible extent of uniformity and harmonization between ICD-11 mental and behavioural disorders and DSM-V disorders and their diagnostic criteria."
with the objective that
"The WHO and APA should make all attempts to ensure that in their core versions, the category names, glossary descriptions and criteria are identical for ICD and DSM."
But the WHO acknowledges that there may be sections where congruency between approved DSM-5 categories and the corresponding categories in ICD-11 Chapter 5, may not be achievable.
For example, the WHO has strict taxonomic rules for ICD classifications and codings which will continue to apply to ICD-11 and which may not facilitate the accommodation of the radical overhaul of the "Somatoform Disorders" section that the SSD Work Group is proposing - even if ICD-11 Revision Steering Group and WHO classification experts were to consider these proposals to be valid propositions.
Between one edition and the next, the WHO may, for example, add new disease and disorder terms; or move an existing ICD category term out of the "R code" chapter (Chapter 18) and relocate it in another chapter in response to scientific developments; or move an existing disease or disorder within a chapter to place it under a different parent class; or remove a parent class, as is being proposed for the G93 Other disorders of brain, for ICD-11.
But the SSD Work Group is proposing to take a number of existing categories (which have parallel categories in ICD-10) and combine them under a new category CSSD, thus:
I consider that ICD-11 would find such radical changes difficult to achieve congruency with under ICD taxonomic rules.
So it needs to be understood that the "Somatoform Disorders" (or "Somatic Symptom Disorders", as they propose to rename them) categories for DSM-5 correspond with the "Somatoform Disorders" categories of Chapter 5 Mental and behavioural disorders in the forthcoming ICD-11 - not with Chapter 6 Diseases of the nervous system, where PVFS, (B)ME have been classified since 1992, and to which CFS is indexed.
It's not known to what extent the various DSM-5 Work Groups (there are 13 plus a number of study groups) and the ICD-11 Topic Advisory Group for Mental and behavioural disorders are collaborating or whether the respective sections of DSM-5 and ICD-11 Chapter 5 are being developed in parallel. It's not known either, at what point in the Timelines for the development of both systems, "harmonization" would be anticipated to have been agreed upon, or rejected if not feasible or acceptable to either party for any given section, for whatever reasons.
But the Alpha drafting platform for ICD-11 currently shows no evidence of mirroring the radical proposals that the DSM-5 SSD Work Group are proposing.
ICD-11 is now running around a year behind with its own Beta draft and has just shifted its Beta Timeline by 12 months, so it's running even more out of synch with DSM-5.
DSM-5 will need to be largely completed by March-December 2012 for presentation to the APA Board of Trustees, whereas ICD-11 isn't now expecting to launch its Beta draft until May 2012 - so the slipping Timelines for ICD-11 and the differences between their drafting and field trial schedules may also present barriers to "harmonization".
DSM-5 is also expected to "harmonize" with the forthcoming US specific ICD-10-CM, for which a partial code freeze will be implemented this year, in October 2011. So the drafting schedules for all three systems are no longer in synch.
You can see the ICD-11 Alpha draft page for "Somatoform Disorders" here:
http://apps.who.int/classifications/icd11/browse/l-m/en#/@_@who_3_int_1_icd_2_F45
(You will need to click the drop down for child classes.)
PVFS, (B)ME and CFS in ICD-11:
For ICD-11 Alpha draft, the proposal is for CFS, PVFS and (B)ME to be classified in Chapter 6, with PVFS -> CFS specified as an Exclusion to Chapter 5 "Somatoform Disorders".
See screenshots for ICD-11 Alpha draft for CFS, showing (Benign) ME specified as an Inclusion term to CFS in Chapter 6 Diseases of the nervous system, plus further notes on the proposals for PVFS, CFS and (Benign) ME in this post: http://wp.me/pKrrB-16N
me.agenda@virgin.net
http://dxrevisionwatch.wordpress.com
http://meagenda.wordpress.com
Readers please note that the CFIDS and MassCFIDS responses that Cort has posted are examples of last year's submissions - not from this year.
There is a new page opened on my site for this year's responses. It is currently empty.
2010 submissions: http://wp.me/PKrrB-AQ
2011 submissions: http://wp.me/PKrrB-19a
UK org, Action for M.E., confirmed yesterday that they are intending to submit again, this year, but as yet, no other UK orgs have confirmed.
Have you found PR's response from last year, yet, Cort? I would be happy to add it to the others on my site.
I am pleased to see that this coaliton of 8 US orgs has now put out a "Call to Action", but it is a pity that this could not have been issued earlier.
My alert and call for action for the second public review period was posted here, on Co-Cure and on my site on 5 May.
There are now only 13 days left.
Why is the American Psychiatric Association referred to in the Coalition4ME/CFS's materials as the "ASA"?
I have copies of last year's submissions on my site for:
International patient organisation submissions:
Whittemore Peterson Institute, Steungroep CFS Netherlands, CFS Associazione Italiana, ME Association (endorsed submission of Dr E Goudsmit), Action for M.E., Invest in ME, Mass. CFIDS/ME & FM, The CFIDS Association of America, Vermont CFIDS Association, IACFSME, The 25% ME Group
Patient advocate submissions:
Suzy Chapman UK (2), Tammie Page M.A. US, Patient advocate US, John Mizelle, Therapist US, Peter Kemp UK, Ian McLachlan UK, Andrew US, Mary M. Schweitzer PhD US
Suzy Chapman
me.agenda@virgin.net
http://dxrevisionwatch.wordpress.com
http://meagenda.wordpress.com
Thanks Suzy - you have really lead the way here - we are indebted to you...
The Coalition4ME/CFS is a bit behind here - we are just learning how to work as a group...In the future we will be quicker to the mark. We hope to leverage our voices to make a strong stand and a real difference in this disorder.
Phoenix Rising will make a submission this year and I will look for our old one.
Other US non-profits are welcome to join.
@ Cort
I do hope you'll be posting a link for this Coalition material in the existing DSM-5 thread:
http://forums.phoenixrising.me/show...SM-5-v.-WHO-s-ICD-in-the-US&p=183871&posted=1
the psych lobby strikes again: DSM-5 v. WHO's ICD in the US
I do hope you'll be posting a link for this Coalition material in the existing DSM-5 thread:
http://forums.phoenixrising.me/show...SM-5-v.-WHO-s-ICD-in-the-US&p=183871&posted=1
the psych lobby strikes again: DSM-5 v. WHO's ICD in the US
Here is PANDORA 2010 letter to APA on DSM5
In addition through our urging Shelley Foote, a clinical psychologist who is associated with the Dade County Psychological Association (DCPA)...shared with PANDORA last year: "Had our DCPA full-day meeting and I am wiped out but I wanted to tell you, despite missing DSM-5' theoretical deadline, I have over 25 letters signed by psychologists expressing their disagreement and disapproval of the CSSD category.I typed out a letter last night, printed it, gave it to them along with your AWESOME letter and a stamped, addressed envelope, how could they say no, right?Just wanted you to know - now go and enjoy the mountain air!!!"
Great to hear about Dr. Foote! Psychiatrists against the CSSD - what could be better than that?
Thanks Suzy - you have really lead the way here - we are indebted to you...
The Coalition4ME/CFS is a bit behind here - we are just learning how to work as a group...In the future we will be quicker to the mark.
Indeed, the DSM-5 issue has been discussed on these forums since December 2009, and I have been publishing on DSM-5 elsewhere since early 2009.
I am a UK advocate and DSM-5 has implications for all of us.
But a US campaign, from the US perspective, needed to have been initiated prior to the last public review, in 2010, or immediately following that review, in readiness for this second review.
It is unfortunate that the APA brought the date of the second review forward - it was originally scheduled for May - June, then shifted to August - September 30, (just one day before the partial code freeze for ICD-10-CM) then reverted to May 4, with no prior warning from the APA. Also, this is a six week review period, whereas last year's was ten weeks - but alerts did go out on May 5, and since then, I have published and circulated two further alerts, and on these forums, too.
I appreciate that the focus has understandably been on XMRV this past 12 months - but however XMRV pans out, there will still be DSM-5, but there has been virtually zero interest in this issue from US patients on these forums since the last public review was held.
me.agenda@virgin.net
http://dxrevisionwatch.wordpress.com
http://meagenda.wordpress.com
I want to ask people to write, but I don't know how to explain why we are responding again. Also, there is a deadline listed. What is the descriptive name of whatever is going on now that will end this month.
Andrew,
The process:
The APA is currently holding
A second public (or stakeholder) review and comment period for its
Proposed Draft Revisions to DSM-IV Disorders and Criteria for new and existing mental disorders.
On May 4, the APA posted revised draft criteria on its DSM-5 Development website for public scrutiny and feedback.
The deadline
The deadline is June 15 - not the end of June. So there are only around 12 days left in which to get comments in.
Registration:
Register on the DSM-5 Development site at any time to submit comment to the appropriate Work Group by June 15.
Comments are uploaded via a WYSIWYG editing tool.
It will accept external links but not attachments. In order to register, stakeholders need to provide name, country and a working email address. On completion of the form, a confirmation email is generated with a password. Last year's log in details appear to have been retained for those who submitted, last year.
You can bring up a commenting box on any page, but I'd suggest that you advise your contacts to respond on this page, once logged in:
http://www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=368
I would also suggest you advise that they head their submissions:
"For the attention of the Somatic Symptom Disorders Work Group"
Also that they state their credentials as a stakeholder, eg, I am submitting comment as a carer, patient, clinician, allied health professional, medical claims lawyer, whatever.
Why are we asking people to comment:
Because we have a second opportunity to submit feedback and make our considerable concerns known. This process is open to all stakeholders and this is an important issue.
Our input and that of professionals may not have any impact but we have this opportunity to submit feedback and we should make good use of it.
The APA says:
http://www.dsm5.org/proposedrevision/Pages/Default.aspx
"The work group members will review all feedback and make decisions about further revisions based in part on the comments provided as well as on results from field trial testing, which is currently underway. Once the next edition of changes have been implemented, we will post the revised criteria on this site to allow commentary once again."
*Please note that all input we receive will be reviewed, though we can not guarantee that your suggestions will be incorporated into any revisions. "
-------
There is a third public review scheduled for January - February 2012, following the field trials. That is currently scheduled for two months.
Since the last public review process, a number of revisions have been made to the proposals for the "Somatic Symptom Disorders" categories and the two key documents have been edited:
http://www.dsm5.org/Pages/RecentUpdates.aspx
[...]
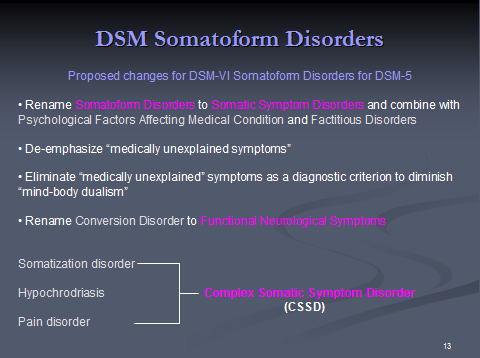
Somatoform Disorders
Addition of the following disorders to DSM-5:
Simple Somatic Symptom Disorder (Ed: that did not appear in the first review)
Illness Anxiety Disorder
Elimination of the following DSM-IV disorders:
Hypochondriasis (being replaced by Illness Anxiety Disorder) Criteria changes:
Body Dysmorphic Disorder - criteria and severity scale updates
Complex Somatic Symptom Disorder multiple changes to criteria and optional specifiers
Conversion Disorder (renamed Functional Neurological Symptoms) addition of criterion D
------------
I don't think we have the two key "Disorders Description" and "Rationale" documents in this thread so I am attaching them.